The Science Behind Autism and the 'Developmental Disorders': Tortuous or Tortured-Juniper Publishers
Global Journal of Intellectual & Developmental Disabilities (GJIDD)
The history of coming to grips with what autism is
and its etiology has been tortuous -if not tortured. By 1908 the word
autism was defined as a schizophrenic who was withdrawn or
self-absorbed. Some decades later Leo Kannern [1]
decided that autism was based on children with "a powerful desire for
aloneness.” In the 1960's psychologist Bruno Bettelheim, picking up on
another aspect of Kanner's [2]
observations, thought autism was simply based upon mothers not loving
their children enough. Then came the twin research studies which
purported autism to be caused by genetics or biological differences in
brain development. Yet the consensus that Autism is from an intrauterine
infection had also been growing, bolstered more recently by Patterson's
[3] and Fatemi's [4]
studies. However, the question would still remain: which infection?
This, of course, remains unknown. Until 1980 autism in the US is still
called "childhood schizophrenia” and in some parts of the world, it
still is. By the same token, there has been, for some time, an extensive
body of medical literature which ties schizophrenia to chronic
infection -some time before when Rzhetsky [5]
in 2007, used a proof-of-concept bio-statistical analysis of 1.5
million patient records, finding significant genetic overlap in humans
with autism, schizophrenia and tuberculosis. Tracing the history of
autism from John Langdon Down's children, a subset of which were
autistic, to the present, this paper also explains how the stealth
pathogen hypothesized to be behind autism has evaded modern day
diagnostics.
Keywords: Autism; Autistic spectrum; Childhood schizophrenia; Asperger's disease; Etiology of autism; History of autism California Department of Developmental Services, Sacramento, 1999
California, in 1999, had been on high alert for some
time. Level one autism, without any of its "spectrum,” went from almost
five thousand cases in late summer 1993 to an estimated 20,377 cases by
December 2002. As California's Department of Developmental Services
stood by incredulously, it witnessed at rippling of California's autism
rate, and all but 15 percent of cases were in children.
California wasn't alone. But its autism rates had
become the fastest growing group in that state's developmental
disability system, and a number of Bay Area school districts were forced
to fill entire classes with youths with different forms of autism.
But even in the midst of California's mini-epidemic,
its Santa Clara County seemed particularly singled out. The Department
of Social Services Aid, brokered by the San Andreas Regional Center,
staggered to its breaking point, and its forecast for autism in Santa
Clara wasn't good.
What was behind this epidemic? A major clue,
overlooked from a critical stand point, was contained in the time line
of the department's own 1999 autism report, which concluded that the
disease had increased dramatically between 1987 and 1998.
What had happened in California in and around 1987 that could haves own the surplus of autism that California no wreaked?
Division of Communicable Diseases, Sacramento, California, 1999
While autism exploded in California, there was also,
beginning in 1987, a major spike in the number of tuberculosis cases
reported by the Tuberculosis Control Branch of California's Division of
Communicable Disease. There, division head Dr. Sarah Royce proclaimed a
TB epidemic in California. The epidemic peaked in1992, had the same male
preponderance as autism, and took off at precisely the same moment in
time.
California's TB epidemic might have already peaked
well before 1999, but this didn't stop it from continuing to contribute
the greatest number of cases to the nation's total tuberculosis
morbidity [6]. But, as with autism, the problem was worldwide, and even the World Health Organization, traditionally slow to
react, had declared a global tuberculosis emergency six years earlier, a warning that has been in existence ever since [7].
Among children, brain-seeking central nervous system
tuberculosis is common in a disease that kills more children each year
than any other, with the potential to cause in survivors, among other
things in its devastating wake, a withdrawal from social interaction [8].
It had to be more than a coincidence, therefore, that
since the 1980s, California experienced a dramatic increase in the
number of children diagnosed with autism as well [9].
Santa Clara County California, March 2006
If California was experiencing autistic rumors, then
surely its Santa Clara County was at the epicenter. By 2006, Santa Clara
had some of the highest rates for autism in the entire country And
although this was for unknown reasons, again the question became, why
Santa Clara? And the answer pointed in a similar direction. By 2002, it
had become apparent that TB was on the rise in Santa Clara, and, by
2006, that county had the highest number of new TB cases in
California-more than most US States. At the same time, the immigrant
share in Santa Clara County, mostly from countries where TB is endemic
was at its highest point since 1870. Santa Clara's Health Department
sounded the alarm. Santa Clara now knew that it had two problems on its
hands. Its medically trained psychiatrists, personnel and statisticians
just never stopped to think that the two problems might be related.
Centers for Disease Control and Prevention, Atlanta, Georgia, September 2008
Time passed. More information came to in. In
September 2008, the Centers for Disease Control and Prevention published
a study by lead author, pediatrician, and researcher Laura J. Christie
of the California Department of Public Health entitled "Diagnostic
Challenges of Central Nervous System Tuberculosis.” Christie and
colleagues identified twenty cases of unexplained encephalitis referred
to the California Encephalitis Project that were indeed tubercular [10].
The team importantly began with the significant statement that
"Tuberculosis (TB) of the central nervous system (CNS)” as thought of by
physicians, "is classically described as meaning it is. However,
altered mental status, including encephalitis is within the spectrum of
clinical manifestations.”
Indeed, according to Seth and Kabra, central nervous
system tuberculosis in children canal so include tuberculous
vasculopathy (infection of cerebral blood vessels), small tubercular
masses called tuberculomas or TB abscesses [11].
In most of the twenty cases, the California
Encephalitis Project culture doubt tuberculosis, the same tuberculosis
considered the least likely cause for encephalitis. Yet there it was.
But, as Christie pointed out, as little as 25 percent of patients with a
diagnosis of CNSTB actually cultured out TB, which was a criteria for
this particular study That means that only %th of possible cases were
being diagnosed. And even the most sophisticated diagnostic lab tests
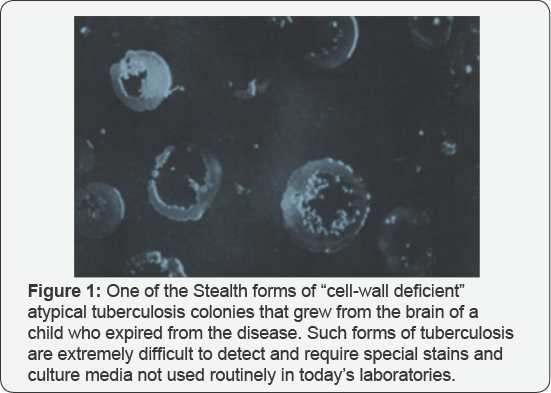
proved not helpful in further probing the culture proven cases (Figure 1).
Office of the Medical Superintendent, Earls Wood Asylum for Idiots, Surrey England, 1887
Figure 2
It was in the teachings of John Lang don Down, some of whose "mentally
retarded” children were autistic, that Leo Kanner really found his
autism. Down, one of the outstanding medical scholars of his day, was
certain to gain entrance into the prominent London Hospital when he
decided instead to pursue an avenue few would entertain, as super in ten
dent of the Earls wood Asylum for Idiots in Surrey. But for Down, it
was preordained. At the age of eighteen, he had what might be described
as a transformative experience. A heavy summer storm drove his family to
take shelter in a cottage. Down wrote: "I was brought into contact with
a fee blamed girl, who waited on our party and for whom the question
haunted me-could nothing for her be done? I had then not entered on a
medical student's career but ever and an on their membrane of that
hapless girl present edit self to mean longed to do something for her
kind”
[12].
Down, therefore, became a doctor for reasons that
were the purist of the mall, and he soon excelled and became the head of
his class. His pursuits were brought to a temporary halt when he
acquired tuberculosis, which sent him back to his family's home in Tor
point. Gradually, here covered. Down then went through an obstetrics
residency before obtaining his MD to assume the position of head of the
Earls wood Asylum. He was now quite knowledge able about pregnancy, the
complications and diseases of pregnancy, and neonates. In addition, his
surgical skills allow him to do autopsies, during which he contributes
much to expand knowledge of conditions of the brain such as cerebral
palsy as well as probe into what had killed the children in his
institution that died from Down syndrome.
In his Let sonian Lectures, Down follows the
psychiatric nomenclature of his time and classifies his most severe
cases of mental retardation in the young under the category of "idiocy”
[13]
. Like Kanner, he specifies that some of his mentally retarded children
had exceptional intellect in specific areas, such as memorization,
music, or mathematics. In fact, a noticeable subset of the autistic
children that Down treated did not appear physically to even have mental
retardation.
Gill berg & Coleman [14] relate that quite a number of reports of individuals with Down syndrome also meet the criteria for autism.
By 1867, John [15]
had appeared in the Lancet, linking childhood mental illness with
tuberculosis. To Down, in fact, children who inherited Down syndrome
"for the most part, arose from tuberculosis in the parents” and not
genetics [16]. Capone mentions that Down's original report attributed the condition to maternal tuberculosis [17].
As a result of such tuberculosis from conception or soon thereafter,
and nothing else, such children's life expectancy would be shortened, as
the same tuberculosis infection would lead to their early demise. The
only thing really wrong with John Langdon Down's theory was that it was
way ahead of its time. He knew that tuberculosis was, as it still is,
the most common cause of death from a single infectious agent in
children, now killing upwards of 250,000 children each year, yet
exceedingly difficult to diagnose [18-20].
He also knew that TB was the single leading cause of death among women
of reproductive age, between fifteen and forty-four, one million of whom
presently die, according to the World Health Organization, each year [21].
Brain and central nervous system tuberculosis account
for 20-45 percent of all types of tuberculosis among children, much
higher than its rate of 2.9 to 5.9 percent for all adult tuberculosis [22].
In fact, tuberculosis of the nervous system has consistently been the
second most common form of TB outside of the lung in the very young. And
of those infants and children who did survive, nearly 20 to 25 percent
manifested mental retardation and mental disorders-serious and long-term
behavioral
disturbances, seizures, and motor (movement) handicaps in addition to
the various other anomalies associated with the autistic spectrum and
what Down called "neuro developmental” behavior problems [23-25] (Figure 3).

Today, Down is considered wrong for saying that Down
syndrome was caused by parental tuberculosis and rather that it is a
"genetic” abnormality, a next a chromo some on Chromosome 21 called
trisomy. But was Done really wrong? To this day, no one has come up with
the actual cause for this genetic abnormality. This was probably why
the discoverer of the extra chromosome, Frenchman Jerome Lejeune,
hesitated to publish results that were otherwise clear- cut. And when
Lejeune faced McGill geneticists at a Montreal Congress of Genetics,
announcing that he had located an extra chromosome in the karyo type of
Down syndrome patients and showed it to them, he was received with
interest but skepticism considerable skepticism. Since, Warthin, Rao,
Lakimenko, and Golubchick have all revealed how tuberculosis itself can
cause chromosomal change reminiscent of those found in Lejeune's trisomy
[26-29].
Warth in showed tuberculosis's early penetration right into the corpus
luteum itself, in which 90 percent of Down syndrome's abnormal meiotic
chromosomal splitting occurs. Rao also found that the tubercle bacillus
is capable of inducing such chromosomal changes as result in Down
syndrome's non disjunction of the human egg. And Lakimenko et al. [30]
independently proved just how devastating TB could be to the
chromosomal apparatus of cell cultures of the human amnion, in tone, but
two independent studies. Each showed an increase in pathological
mitoses, arrest of cell division in metaphase, and the actual appearance
of chromosomal adhesions absent in control cultures. Indeed, Lakimenko
et al. [30]
demonstrated that early tubercular involvement was not only destructive
against chromosomes but the very spindles that separated them. Total
ovarian destruction occurs in 3 percent of women with pelvic
tuberculosis, against the site where Down syndrome's and autism's
chromosomal abnormalities usually occur[30].
For his Lancet study, Down submits one hundred post
mortem records of children who had passed away at his institution. He
had found no fewer than 62 percent of these children to have tubercular
deposits in their bodies. For some unknown reason, boys had more than
twice the incidence of tubercles in their organs as did girls, a finding
that concurred with the male predominance he later notes in childhood
mental disease in general. Such male preponderance is today not only
documented in Down syndrome but in autism as well. Tuberculosis is might
be more frequently transmitted by the mother than the father, but it
was the male offspring who were more tubercular. Caldecott, in a 1909
British Medical Journal article, noted that Down showed that the
children in his study rarely lived beyond twenty years as a consequence
of brain and nervous system disease, and that they died of tuberculosis [31].
Department of of Psychiatry, Burgholzli Hospital, Zurich, Switzerland, 1930
Figure 4
The word autism first appeared in English in the April 1913 issue of
the American Journal of Insanity, heralded at an address that Swiss
psychiatrist Paul Eugen Bleulerde livered for the opening of Johns
Hopkins University's Henry Phipps Psychiatric Clinic [32].
Bleuler used the word autism, Greek for "self,” to
describe the difficulty that people with schizophrenia experience
connecting with other people, and, in certain cases, with drawing into
their own world and showing self-centered thought. But to Bleuler,
schizophrenia, and there by autism, still came from an organic cause
such as infection, and, as such, was sometimes curable. Until about
1980, autism and schizophrenia were considered basically one and the
same. To that point, Bleuler's definition holds.
Bleuler also uses autistic to describe doctors who
are not attached to scientific reality, wont to build on what Bleuler
calls "autistic ways” that is, through methods in no way supported by
scientific evidence, an event more and more in evidence as psychiatrists
moved away from tissue-based out comes into the realm of subjective
behavioral belling. The history of autism would seem any such
individuals. "Bleuler used the word autism, Greek for "self,” to
describe the difficulty that people with schizophrenia experience
reconnecting with other people, and, in certain cases, withdrawing into
their own world and showing self-centered thought.”
Child Psychiatry Service, Johns Hopkins University Hospital, Pediatric Division, Baltimore,1933
Internal-medicine trained Leo Kanner [1]
teaches himself the basics of child psychiatry and, at the instigation
of Adolph Meyer, joins the Henry Phipps Psychiatric Clinic at John
Hopkins Hospital in Baltimore.
By 1903, Henry Phipps, wealthy partner of Andrew
Carnegie, sought charitable outlets for his wealth. He then joined
Lawrence F Flick, a doctor with a vision, to open a center solely
dedicated to the study, treatment ,and prevention of tuberculosis, hands
down the number one infectious killer in the United States.
Figure 5
Not until May 1908 did Philadelphia steel magnate Phipps get around to
visiting Johns Hopkins's tuberculosis division, which he had funded. At
that point Phipps turns to ask John Hopkins's dean and legendary
pathologist William Henry Welche if he needed help sponsoring other
projects at the Hospital. Welch answers Phipps by handing him a copy of A
Mind that found itself, an agonizing assessment of mental asylums
written by Clifford W Beers and published with the help of Swiss born
pathologist Adolph Meyer [33].
Within a month, Phipps agrees to donate $1.5 million to fund a
psychiatric clinic for the Johns Hopkins Department of Psychiatry. By
1912, the Henry Phipps Psychiatric Service at Johns Hopkins Hospital
provides the first in-patient psychiatric facility in the United States
for the mentally ill. Welch likes Meyer. Meyer, although unable to
secure an appointment from his all matter, the University of Zurich, is,
like Welch, a pathologist a neuropathologist to be exact. Also Welch
takes to him because Meyer initially seems to reject Freud as the be-all
and end-all for psychiatry. And there is another level of
understanding: Meyer and Welch share the rapport of two superb medical
networkers and politicians. Welch sees to it that Meyer becomes the head
of psychiatry at Johns Hopkins.
But it is the very same second-rate, vague,
"psychobiological” views that characterize Meyer's psychiatric approach
that will prove in the end to be disappointing. Designed to be all
things to all people, Meyer's psychobiology assesses mental patients’
physical and psychosocial problems concomitantly, but turns out to be
all things to no one. Meyer is much more oriented towards taking
extensive histories of his patients; getting all the "facts”, then in
rooting out the pathology behind mental illness son the autopsy table.
Besides, the positions of Meyer and Freud closely resemble one another
in that each insists heavily on the study of psychogenic factors in
neurotic disorders. Welch, on the other hand, was committed to bringing
the German model, which relied heavily on the lab, to US medicine. So
with Meyer, Welch didn't precisely get what he thought he was getting.
Nevertheless, thanks to neurologist and pathologist Adolph Meyer, Leo Kanner [1]
becomes the first "child psychiatrist” at Johns Hopkins and, by
default, in the United States. Meyer is Benton changing American
psychiatry, and will dominate psychiatry from his Johns Hopkins chair
during the first half of the twentieth century. Meyer has long been
interested in the psychiatric treatment of children, so hear ranges with
Johns Hopkins pediatrician Edwards Park for Kanner to become aliasion
between pediatrics and psychiatry at the institution. This gives Kanner
enhanced influence in reaching an audience of pediatricians who
otherwise would have found little value in the psychiatric evaluation of
children. Meyer has already decided that the psychosocial aspects of
mental disease are more important than tissue diagnosis of brain
pathology. He closes his laboratory, and instead prefers talking to his
patients, taking extensive histories in the manner of Kraepelin and
Sigmund Freud.
Child psychiatry service, Johns Hopkins University Hospital, Pediatric Division, Baltimore,1934
(Figure 6)
Kanner, with little use for medical diagnostics himself, seems made to
order for Meyer. Kanner will and Meyer for shifting the emphasis of
psychiatry "from organs and their diseases to patients as improperly
functioning persons [34].”
But diseased organs can themselves lead to improperly functioning
persons. Kanner never really seemed that interested in "organs and their
diseases”. While still in Berlin finishing his medical education, his
lowest grade on his finals is as the result of being unable to diagnosis
the then premier infectious brain disorder leading to mental symptoms.
Neurologist Karl Bonhoeffer documents that Kanner misinterpreted the
symptoms of tabesdorsalis, a neurologic end-stage syphilis of the brain
and nervous system [1].
Not really attracted to being a general internist, and still in Berlin,
Kanner gravitates into the then new and relatively limited field of
electrocardiography, or EKG tracings of the heart's rhythms. Once at
Johns Hopkins, Kanner writes his first edition of Child Psychiatry in
1935, borrowing the name from the German term Kinder psychiatric. And by
1943, bent upon making his mark, he discovers a "new” syndrome. Without
mention of Bleuler, who originated the word "autism”, Kanner use sit to
describe what he feels to be a novel psychiatric illness in children,
emphasizing an "autistic aloneness” and "insistence on sameness.”
Ironically, Kanner, known to rant and rage over mere psychiatric labels
without treatment, creates another one: autism.
Office of the Director, Department of Medical Genetics, New York State Psychiatric Institute, July 1936
(Figure 7)
Leo Kanner and Franz J Kallmann had a couple of things in common. Both
had connections with the University of Berlin. Kallmann worked for four
years at Berlin's psychiatric institute under the same Karl Fried rich
Bonho effer who graded a portion of Kanner's final exams. Although
Kanner is only three years older than Kallmann, and Kanner is trained in
internal medicine, both would move quickly upon their arrival to the
United States to make their impact on psychiatry Landing in New York,
Kallmann establishes the Medical Genetics Department of the New York
State Psychiatric Institute. From the no, one thing is certain: With
Franz J Kallmann, American psychiatry got much more of the hereditary
patterns in mental disease than it was willing to accept or pursue.
Prominent British geneticist Penrose judged Kallmann's work
unconvincing. A year after Kanner writes Child Psychiatry, Kallmann
becomes interested in twins and their genetic disposition. But there
arises an inconvenient truth: Identical twins, who have virtually the
same DNA, do not always develop the same mental disorders. Kallmann
focuses on what he calls the "genetics of schizophrenia.” In a lecture,
he finds it desirable to prevent their production of relatives of
patients with schizophrenia. He defines them as undesirable from
aeugenic point of view, especially at the beginning of their
reproductive years. By 1938, Kallmann, who escaped Nazi Germany because
he was half Jewish, has doubled down, calling for the "legal power” to
sterilize "tainted children and siblings of schizophrenics” and to
prevent marriages involving "schizoideccentrics and border line
cases.”In his mind, Kallmann feels the need to stamp out every recessive
gene behind schizophrenia [35].
It was a thought that began incubating in him while he was still in
Germany LeoKanner is appalled by Kallmann's thoughts and words. He sees
dangerous implications. This time he is correct. Kallmann is a zeal at
in every sense of the world. He finds a genetic basis for just about
everything. He proclaims that human tuberculosis is genetically based.
His age is doing so is quite transparent. Proponents like Kallmann for a
"genetic” or "hereditary” view of mental illness have always relied on
identical twin studies. In these, if there is a heavy degree of
"concordance”-meaning that if both identical twins comedown with the
illness-it is supposed that "genetic” influences are involved. This is
so, especially if at the same time fraternal twins show a much lower
rate in being "concordant for”-or contracting-the same disease. But it
was also known that an infectious disease like tuberculosis brought in
the same numbers in identical twin studies as did schizophrenia or
autism, putting the accuracy of such twin studies deeply in question. In
fact, it was Kallmann himself who found that approximately 85percent of
identical (homozygous) twins had the same disease (were concordant) if
their co-twin had either tuberculosis or schizophrenia [36,37].
Kallmann's study for the hereditary basis of schizophrenia is published
in 1938. It acknowledges his long-time boss and Nazi mentor Ernst Rudin
[38].
While still in Germany, Kallmann saw Rude in catapulated to director of
the Kaiser Wilhelm Institute for Psychiatry and it's eugenics division
through Rockefeller Foundation money, creating the medical specialty
known as psychiatric genetics.
Rudin was not only assisted by Kallmann but another proto gene named
Otmar Verschuer. Back in Germany, Rudin, a year later, sees to it that
the German version of Kallmann's book is used by the NaziT4 Unitasa blue
print for the murder of mental patients and "defectives,” many of them
children. 250,000 are killed under this program, by gas and lethal
injection. The Rockefeller-Rudin operation had become a section of the
Nazi state. Rudin was now head of its Racial Hygiene Society. Mean
while, in the United States, geneticist Franz Kallmann becomes an early
leader of the American Society of Human Genetics, a true pioneer in the
study of the genetic basis of psychiatric disorders. Kallmann's American
Society of Human Genetics organizes the Human Genome Project. The most
ambitious project ever dealing with basic genetics. In 1988, Congress
provides funds for the National Institutes of Health and other groups to
begin mapping out human DNA. The project began officially on Octoberl,
1990, with a projected budget of $3billion over the next fifteen years.
As BW Richards points out, advances regarding the discovery of genetic
markers for diseases such as autism, Down syndrome, and schizophrenia,
although good for diagnostics, have done little to get at the actual
cause of such chromosomal aberrations. Richards: "Despite dramatic
advances in the fields of biochemistry and cyto genetics, revealing many
new causes of mental retardation, a large proportion of mentally
retarded patients are still un diagnosable in respect of etiology
(cause)”[39].
What did result, thanks to such take-no prisoners actions like
Kallmann's, was that bacteriology was purposely confined to a special it
of medicine outside the schools of biology, botany, and zoology, in no
small part responsible for bacteriology's slow acceptance.
Bacteriologists, in retaliation, steered clear and gave no credence to
any of the proclamations of geneticists. Unbelievably, the situation had
gotten so out of hand that, as late as 1945, bacteriologist Rene Dubos,
discoverer of the first Antibiotic ever, had to muster all of the
courage in him to name his mile stone paper "The Bacterial Cell.” Such
are and always have been the politics of medicine.
Office of the Director of Child Psychiatry, John Shopkins Hospital, Baltimore, 1943
(Figure 8)
To make certain that his theory sticks, Kanner cherry-picks eleven
children, leaving out those presently with seizures or mental
retardation even though these are very much in today's autistic
spectrum. Some studies have mental retardation occurring in
approximately two-thirds of individuals with autism and seizures in
approximately one-third.
Kanner produces a thirty-three-page medically sketchy paper [2].
He outlines eleven case histories, all the while convincing himself
that, despite findings such as a history of seizures, which could point
to a brush with serious disease, his subjects' problems were purely
psychiatric or behavioral. At the same time he says that, unlike
childhood schizophrenia, autism is the result of "inborn autistic
disturbances of affective contact”-a kind of congenital lack of interest
in other people. Yet most of his children are thought to be deaf,
neither talking nor responding if questioned, and could have severe
cranial nerve disruption from a previous or present serious central
nervous system infection. "Physically,” Kanner insists, despite findings
that suggest otherwise, "the children were essentially normal.” But
five out of his eleven subjects, through measurement "had relatively
large heads,” which could indicate possible degrees of hydrocephalous.
Hydrocephalous, also known as "water on the brain,” is a medical
condition in which there is an abnormal accumulation of cerebro spinal
fluid in the ventricles, or deep cavities, in the brain. This may cause
increased intracranial pressure inside the skull and progressive
enlargement of the head, seizures, and mental disability. Not uncommon,
one of its causes in infants is perinatal infection affecting the brain
and nervous system. At one time, the diagnosis of acute hydrocephalus
was so commonly associated with tuberculosis meningitis that the terms
were used interchangeably. But apparently of more concern to Kanner were
the children's parents: "In the whole group, there are very few really
warm hearted father's or mother's.” Kanner in general felt that
disturbed children often were the product of parents who were highly
organized, rational, and cold, "just happening to defrost enough to have
a child” [40].
When, in his first case, Kanner finds out through DonaldT. Mother that
the child had been placed in a "tuberculosis preventorium” for "a change
of environment,” Kanner never questions her as to why, but notes that
while in the tuberculosis preventorium, he exhibited a "disinclination
to play with children. ”Kanner will later relate that "the mother gave
Donald little attention because "she feared he would give her
tuberculosis” and casually dismisses this by adding, "which he did not
have” [41].
But in order to be sent to a preventorium, Donald T. Must have had a
positive TB skin test, which was not mentioned; nor was it mentioned
what other tests were performed to rule out that the child did indeed
not have tuberculosis.
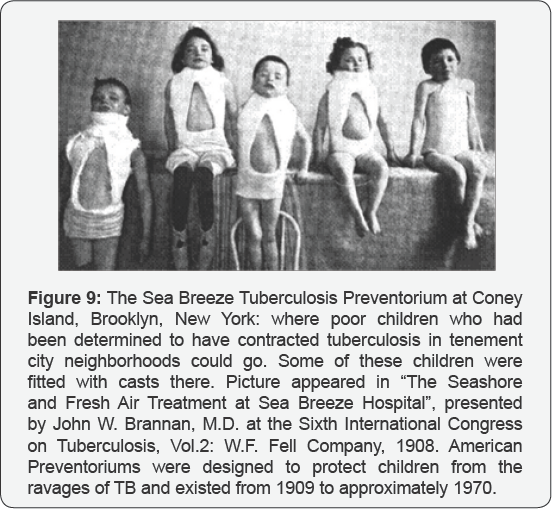
Figure 9
all but forgotten, tuberculosis preventoriums were America's answer to
preventing tuberculosis epidemics among the urban poor. This was
accomplished by ripping "pretubercular” children from their homes and
placing the mint of residential institutions [42].
From the beginning of the twentieth century and well into it, such
primitive "preventoriums” were seen as the only solution to break the
chain in a disease that, by 1900, had killed at least 15 percent of
urban populations, with no treatment in sight. By 1907, von Pirquet came
up with a children's tuberculin skin test with all the flaws of our
present adult tuberculin skin test. Not only were false negative tests
done on seriously infected children whose immune systems could simply
not muster a positive skin reaction, but even when the test proved
positive, it was often impossible to distinguish mere previous exposure
from active disease. Nevertheless, the imprecise designation "pre
tubercular” was used to designate children with positive skin tests who
didn't seem to have active disease. These were the children targeted for
preventoriums. Kanner knows from the onset that his definition of
"autism” will be challenged, on many levels. Even among psychiatrists
presented with these same children, responses would include mentally
retarded or schizophrenic. The fact was that, psychiatrically, all would
be considered by many as having a form of childhood schizophrenia. To
make the differentiation stick, Kanner emphasizes "extreme solitude from
the very beginning of life” and a preserved intelligence. But many of
the developmentally disabled children that Down had studied had normal
intelligence also and certainly did not appear to have mental
retardation [43].
Kanner argues that the children in his study, unlike schizophrenics,
did not seem to have elusions or hallucinations. In addition, he says,
schizophrenia doesn't emerge in as early as the thirty months after
birth that autism seemed to. But more tellingly, in 1949, Kanner
vacillates, admitting that he sees none for his "infantile autism” to be
separated from schizophrenia [2].
The American Psychiatric Association (APA) balks in accommodation and
decades later still won't acknowledge autism as anything other than just
that: "schizophrenia, childhood type.” [44] By then, Kanner deplores the APA's decision [1]. Yet despite this, until 1980, Kanner's autism is not autism; it is childhood schizophrenia [45].
One year after the APA's 1968 decision, prominent Bellevue child
psychiatrist Lauretta Benderargues that children with autism generally
grow up to have schizophrenia any way. And on top of that, despite the
ever-increasing rallying cry by American psychiatric guru's as to
childhood schizophrenia's extreme rarity, Bender documents thousands of
cases of it while at Bellevue [46].
German psychiatry, which long maintained its influence over Europe, and
the Soviet and Eastern Bloc countries also insisted that childhood
autism is the initial form of schizophrenia, with development into
schizophrenia more or less in evitable. Moreover, some in the field
understood that clear and unmistakable evidence of the autistic disorder
could be found in J Langdon Down's 1887 "developmental” form of mental
retardation, which Down attributed mostly to tuberculosis in the child's
parents [13,16]. The stage was set for a battle royal.
Johns Hopkins Department of Pathology, Baltimore, 1946
Though his office was but a short distance away from
Leo Kanner's, Johns Hopkins TB pathologist Arnold Rich lived in a
completely different world. In Rich's world, there were no psychiatric
hypotheticals, no diagnoses not verifiable by laboratory reagents and
microscopic findings.

Figure 10
Although it appeared that Rich and Kanner worked in completely
different arenas, at times they unknowingly touched directly on one
another's work, but never more closely than when Rich began to focus on
perinatal infectious disease. Rich was a teaching dynamo at Johns
Hopkins, completing his authoritative Pathogenesis of Tuberculosis in
1944, with a second edition in 1951 [47]. It took him nine years to compile and still remains a model of what a scientific monograph should be.
By virtue of his astute powers of observation, Rich
had always stood out from the rest, even at Johns Hopkins. His name
remains on the lung condition called Hamman-Rich syndrome, and the small
tuberculousmasses (tuberculomas) that metastasized, not in frequently,
to, among other areas, the human brain, and became immortalized as
"Rich's foci”. He was also the first to describe the high prevalence of
occult prostate cancer in elderly men as well as the first to describe
wide spread vascular obstruction in the lungs in children with the
hereditary heart condition called Tetralogy of Fallot.
During Rich's tenure, much as in the past, the
prevailing emphasis at Johns Hopkins laboratory research was either with
the living or recently deceased, but the way in which Phipps psychiatry
under Meyer neglected it's bench work research gave it a somewhat
remote character to the rest of Johns Hopkins, preventing closer
association. In addition, it seemed that Meyer's protege, Leo Kanner was
looking only at the very tip of the same iceberg that John Langdon Down
had come to grips with so long ago. When Kanner spoke of an "inborn”
condition affecting mentation, Rich, as well as Down previously, had
afairly good idea of what he was speaking about, and to Rich it was no
more a condition caused by heredity than the nonsensical documents that
crossed his desk weekly claiming human TB to be hereditary or caused by
the wrong genes. Rich, like Down, knew that TB was the most common cause
of death from a single infectious agent in young children and neonates,
commonly attacking their central nervous system [18, 48].
The Germans had their own name for childhood tuberculosis, kinder
tuberculose, and in the many children who survived, besides leaving
their tiny bodies gnarled, nearly 20 to 2 5 percent manifested mental
retardation and psychiatric disorders [23].
And for various reasons, many did survive-leaving in its wake, among
other conditions -Down syndrome, the autistic and the 'mentally
disabled'. So until this significant pool of infected neonates, infants,
and toddlers was fully evaluated for such protean mental complications,
Arnold Rich truly couldn't understand psychiatrist's fussing over
"inborn” features of a "psychiatric” disease, whether labeled autism or
anything else that very possibly was caused by organic infection. It
just didn't make sense. A neurologist friend had confided in Rich that
Kanner's autism seemed more like a disease caused by post-encephalitic
phenomena than anything else. Rich knew that tuberculosis was fully
capable of causing such an encephalitis, described by one pediatric
infectious disease specialist as being indolent or slow to develop and
heal, often as painlessly as any other central nervous infection around [49].
Figure 11
Rich looked up at the picture of William Henry Welch (1850-1934). Welch
had been both Rich's predecessor at Hopkins Department of Pathology, as
well as dean of medicine and founder of the Johns Hopkins University
Medical School. Welch was unique. Welch was different. He was an over
and a shaker, an organizational genius who would single-handedly force
US medicine up to and eventually beyond what they had in Europe. A
bacteriologist and a pathologist, Welch would one day be called the dean
of American medicine. During his watch American life expectancy would
jump by at least twenty years. And William Henry Welch would be a major
factor in that leap.

Rich looked up at the picture of William Henry Welch (1850-1934). (Figure 11)
Welch had been both Rich's predecessor at Hopkins Department of
Pathology, as well as Dean of Medicine and founder of the Johns Hopkins
University Medical School. Welch was unique. Welch was different. He was
an mover and a shaker, an organizational genius who would
single-handedly force US medicine up to and eventually beyond what day
be called "the Dean of American medicine" During his watch American life
expectancy would jump by at least twenty years And William Henry Welch
would be a major factor in that leap.
Rich was proud both of the association and to have
personally known the physician considered both the father of American
medicine and one of its most influential members. Welch had studied in
Germany under the great masters, including stints with Koch, Cohnheim,
and psychiatrist and neurologist Meynert. Welch therefore well realized
the importance of seeking out diseased tissue in the mentally ill.
Meynert decried those like Kraepelin and Meyer, who Seemed preoccupied
with labeling symptoms instead of going after the real tissue cause of
brain or central nervous system illness [50].
And having also worked with Koch, Welch held a keen appreciation for
the destruction, both inside and outside of the mind, that tuberculosis
could cause. With regard to the immediate problem in front of him, Rich
had read Knoph's review in which he said of Welch that "He too was of
the opinion that a direct bacillary transmission, that is to say,
prenatal infection (with tuberculosis), takes place much more frequently
than believed”[51].
Like Rich, Knoph also knew that few fetal autopsies
and exhaustive studies were done to prove fatal tuberculosis on dead
fetuses. And those studies had to contend with the fact that
tuberculosis, a microbe that grew only with sufficient oxygen, was most
often impossible to isolate in the low-oxygen content of fetal blood or
tissue. It's not that TB had any trouble surviving under low-oxygen
conditions; it just did so in undetectable dormant forms, causing a
diagnostic night mare. Rich questioned the wisdom of Welch in choosing
someone like Adolph Meyer to run Hopkins's psychiatry. Meyer seemed such
a far cry from Johns Hopkins neurologist D.J. Mc Carthy, previously on
staff at Phipps Tuberculosis and an authority on tuberculosis of the
nervous system in infants and children [52].
McCarthy knew not only that cerebral tuberculosis occurred with much
greater frequency in infancy and childhood than most realized, but
reported a distinct and causative relationship between tuberculosis and
adolescent schizophrenia itself. In fact, McCarthy's investigation at
Johns Hopkins Phipps Tuberculous Pavilion for the mentally ill revealed
that practically all of the patients isolated there had schizophrenia.
This seemed particularly relevant when taken in light of Lauretta
Bender's argument that children with autism generally grow up to have
schizophrenia anyway [46].
McCarthy was far from the first investigator to link schizophrenia with
TB. Although eventually the term childhood schizophrenia was displaced
altogether regarding autism, there remained those children who displayed
both the early-appearing social and communicative characteristic of
autism and the emotional instability and disordered thought processes
that resembled schizophrenia. Rich wondered if either Kanner or Meyer
had as extensive a knowledge of the infectious orientation of German
psychiatry as did pathologist William Henry Welch, who once walked with
its giants.
Psychiatric Asylums on the European and American Continents, Late Nineteenth Century
When Johns Hopkins pathologist William Henry Welch
studied under psychiatrist Meynert, it was in the late nineteenth
century, a time off earth at tuberculosis would destroy the entire
civilization of Europe. It was also when the first massive increase in
psychiatric illness and confinement to mental asylums occurred [53].
And although there was a sociological shift of patients going from
family care and poor houses to asylums, this in itself could not account
for the inexorable increase in asylum census. To distinguished
psychiatrist and writer E. Fuller Torrey, severe psychiatric illnesses
such as schizophrenia were comparatively new diseases, less than 250
years old, the confinement for which, even as a college student,
reminded Torrey of the tuberculosis sanitariums of a slightly earlier
era [54].
During this time frame, there was no autism as understood by Kanner,
just the autism Bleuler used to describe schizophrenia. Nor was there
the capacity to do a proof-of-concept bio-statistical analysis showing
significant genetic overlap in humans with autism, schizophrenia and
tuberculosis. Rather autism and schizophrenia were simply considered as
one with infectious concepts brought forward still being revisited by
various author's today [5,55].
In nineteenth- century asylums, the upward spiral became obvious. By
1884, in Germany, Karl Kahlbaum, perhaps the most under rated
psychiatrist in history and the true originator of US outcome- based
psychiatric classification, first described schizophrenia as a separate
entity. Kahlbaum: "It must be the experience of all psychiatric
institutions that the number of youthful patients has recently undergone
a considerable increase” [56].
It was between 1700 and 1900, that tuberculosis was responsible for the
deaths of approximately one billion (one thousand million) human
beings. The annual death rate from TB when Koch discovered its cause was
an incredible seven million people per year. There were others who also
saw this nineteenth-century grounds well of mental illness as
representing something new, including auditory hallucinations, as never
witnessed before.
Historians like Hare and Wilkins, among others, point out that it was
only then that schizophrenia, with its hallucinations and delusions, was
really even mentioned, representing no small part of the
late-nineteenth-century psychiatric flare ups [57,58].
Almost unheard of in the medical literature before this, chronic
delusions and hallucinations-such as hearing voices-became common in
asylum admissions at the same time Clouston, by 1892, was documenting
them in mental illness as a result of a killer pandemic of tuberculosis [59].
Max Jacobi, the originator of the school of thought that held that
infectious illness led to mental illness, was the first to a scribe
characteristic symptoms for this associated with tuberculosis [60].
Just as autism was thought to be a disease of "affect” or emotion by
Kanner, Jacobi in particular considered an unpredictable, emotional
(affective) change ability as characteristic of, and at times even
diagnostic for, latent, undiagnosed TB. Incredibly, Grading found
pulmonary tuberculosis during autopsy in 70 percent of mental defectives
and in 50 percent of the mentally affected with seizure disorders [61]. Seizures, not uncommon in autism, occurring 20 to 30 percent of its patients based on the majority of studies [62].
Barr spoke about the relationship between tuberculosis and mental
defectiveness at the Sixth International Tuberculosis Congress held in
Washington, DC, in 1908 [63].
There, Jacques More expressed his belief that epilepsy and the
convulsive disorders were derived from tuberculosis. A year previously,
An glade spoke not only on how tuberculosis caused epilepsy in infants
and the young, but how such epileptics eventually became mentally
defective through sclerotic brain changes caused by the disease [64].
Subsequently, Baruk discovered that when either proteins extracted from
tuberculosis or the spinal fluid taken from people with schizophrenia
were introduced into healthy animals, a condition called catalepsy
occurred, in which the body and its functions seemed frozen in time.
Catalepsy is associated not only with one form of schizophrenia but with
epilepsy itself [65].
Patients with catatonia, an extreme form of withdrawal in which the
individual retreats into a completely immobile state, can also exhibit
catalepsy. Wing related in 2000 that the incidence of catatonia could be
as high as 17 percent in adolescents with autism [66].
Historically prominent Viennese pathologist Ernst Lowen stein decided
to take things a step beyond. Having developed a potato flour-and
egg-based tuberculosis growth media, still in use today, he set about to
prove that TB could be cultured from the blood of patients with
schizophrenia [67].
Yet despite nine independent confirmative studies finding either the
tuberculosis bacillus itself or it's much harder to stain yet more
common viral forms, other studies couldn't confirm these results.
Whether this was from defective laboratory procedure or from the
difficulty in staining and culturing viral (or cell-wall- deficient
forms) of tuberculosis remains, to this day, unknown. What is known is
that undeterred and in answer to these negative studies, Weeber, Melgar,
and Löwen stein again found tuberculosis in the blood of schizophrenic
patients-findings which, to this day, remain un addressed [68-70].
As far back as 1769, Scots man Robert Whytt, reporting on approximately
twenty cases, described the localization of tuberculosis in the
meninges, membranes that cover the brain and spinal cord [71].
Realizing that the localization of tuberculosis there was often
associated with mental disturbances, Whytt gave us the first description
of tuberculous meningitis, at that time called morbuscerebralis
Whyttii. In describing the disease, Whytt noticed not only small masses
called "tubercles” in the brain tissue but hydrocephalus, an excess of
"water in the brain.”A duct system circulates fluid in the brain and
spinal cord. The meninges that cover the brain manufacture and contain a
cerebro spinal fluid that circulates through channels of deep cisterns
in the brain and then down the spinal cord and back to the brain. A
block in this circulation, whether from a congenital condition or
disease, can lead to an increase of cerebrospinal fluid around the
brain. In infants and young children, because the bones of their skulls
are still unfused, this can result in an enlargement of the head. No
matter the age, mental disturbances and even retardation can result as
complications of such hydrocephalus. So inter twined was hydrocephalus
with tuberculosis that medical experts by the end of the nineteenth
century considered acute hydrocephalus as just another name for
tuberculous meningitis [72].
Since 1854, Wunderlich recognized that psychotic episodes, including
schizophrenia, could be caused by small masses of tuberculosis
(tubercles) in the brain [73].
But only as time passed, did it became more obvious just how commonly
this occurs. The tubercles of tuberculosis, which often form masses
called tuberculomas, are launched through the blood stream to the brain
and are often found in infants and adults with no neurologic symptoms.
But Marie documented symptomatic cases of tubercles as a cause of
psychosis such as schizophrenia [74].
TB meningitis was just the tip of the iceberg, and other investigators,
as early as 1908, uncovered a more generalized inflammation of the
brain matter, tuberculous encephalitis, "as also being behind specific
psychosis [75]. So the term tuberculous meningo encephalitis was considered more accurate than just tuberculous meningitis.
Department of Pathology Johns Hopkins, 1948
Arnold Rich was working on a problem that might have
major implications toward Kanner's child psychiatry, but he was having a
problem with regard to the frequency of maternal-to-fetal transfer of
tuberculosis [47].
It was also an issue with seminal significance in addressing Downs
develop mental disorders, of which autism was a division. In fact, it
was a topic that had been addressed by some of the greatest minds in
medicine. On the one hand, Rich knew that "It is now well established
that tuberculous infection can be transmitted from mother to fetus
through the placenta.” He references Warthin, who in an article in the
Journal of Infectious Diseases, said it was common, and Siegel's study
in the American Review of Tuberculosis [26,76].
Siegel documented infants that had died from the disease, one or two
days after birth. Husted's study even included tubercular still birth [77].
Figure 12
But to further establish the importance of a link between maternal and
perinatal tuberculosis, Arnold Rich felt the need to go into the numbers
involved in the general population. Of all the infectious diseases, TB
was and always had been a disease of alarmingly large numbers. Ever
since Norris's original review, it had been known that, for some reason,
pregnancy, especially late pregnancy, and child bearing itself
dangerously re-animated any form of tuberculosis in a woman's body, no
matter how silent [78].
Even latent TB with no symptoms, Norris mentions, could reactivate,
percolating TB bacilli in to the maternal blood stream for transfer into
the fetus. Thus, in the first half of the twentieth century, the method
of choice for an expectant mother with proven TB was early termination
of pregnancy [79].
Menstruation itself had a similar deleterious effect, causing its own
flare up of tuberculosis in the body. The numbers in front of Rich were
incredible.
In a disease that, according to the World Health
Organization, consistently kills more women of child bearing age than
any other, the age at which female tuberculosis mortality began to rise
above male mortality coincided with the average age of the onset of
menstruation. But the age at which the rate of tuberculosis mortality
really surpassed that of males coincided with the period during which
over two-thirds of all pregnancies occurred. Rich conservatively
estimated that a little over two million women between the ages of
eighteen and thirty were pregnant in 1940. And since the total US
population for women of this age was approximately 17.7 million, it
followed that one out of every eight women in the United States was
pregnant in this age range, and one in ten bore living children. This
not only produced a pool of 200,000 opportunities to re animated and
often undiagnosed maternal tuberculosis, with its drastically increased
female mortality rate, but, with such reactivation, the possibility for
the transmission of that disease to the fetus and newborn. In such are
animation of latent tuberculosis, it was also striking that TB
meningitis-which is in frequent in adults but frequent in infants and
toddlers-seemed to also noticeably increase in childbearing women from
there activation of old deposits of cerebral tuberculosis [80].
Rich already realized that, regarding TB's fatality in neonates,
infants, and young children, there was a definite pattern. Tuberculosis
was most fatal during the first year or two of life. After the second
year, the death rate for infected toddlers fell markedly, probably
through a greater ability to form protective antibodies between the ages
of two and five than during infancy [81].
Though the disease was still deadly for the remainder of the first five
years, by far the safest period was between five years and puberty,
when the death rate from TB plummeted. Often termed the "golden age of
resistance,” for some reason, children between ages five and fifteen are
more resistant to TB than adults and infants. It was an interesting
fact, creating a possible theoretical under pinning for Bender's
assertion as to how autistic involvement in the very young, hardest hit
in the first thirty months, could come back as a related schizophrenia
during adolescence, toward the end of the period of remarkable
resistance to the disease. It was thought at one time that newborns were
completely devoid of resistance to tuberculosis [82].
But sufficient studies had since contradicted this notion. In Brailey's
study at Rich's own Johns Hopkins Hospital, of sixty- five infants who
became tuberculin positive during the first year of life, two-thirds
were alive and well at the end of five years [83].
So the acquisition of tuberculosis by infants was not necessarily a
death sentence. However, its complications, including those involving
the brain and nervous system, could soon impact the individual for the
rest of his or her life. As to whether a notun common tuberculous focus
in the brain killed, Rich would soon find, was a matter of what he could
only refer accurately to as what card players know as 'the luck of the
draw'. It is not generally appreciated that the development of small,
rounded nodules caused by tuberculosis, sometimes cheesy or "caseous” in
the brain, is a relatively common occurrence in children and childhood
tuberculosis. It is usually symptom less. Such small nodules often
become arrested and encapsulated by the body's immune system. They are,
to this day, called Rich's foci. Many of us unknowingly have them. But,
stressed Rich, it is when small tubercle nodules happen to land in that
part of the surface of the cerebral cortex ear the meninges (covering of
the brain),no matter how small, that serious troubles began. Such
infectious nodules often extended into this protective covering through
which cerebro spinal fluid percolates on its journey through the brain
and into the spine. Such a discharge of tuberculosis into the spinal
fluid of the meninges (in its subarachnoid space) can (and often does)
lead to potentially fatal meningitis. The disease festers and spreads
throughout the central nervous system. There need not be extensive
infection, just one tiny nodule in the wrong place, near the meninges.
On the other hand, the development of small tubercles deeper in the
brain substance, though relatively common, often gave rise to no
symptoms what so ever. Rich himself had seen one-inch tuberculous masses
lodged in a silent area of the brain that were seemingly entirely
harmless. As ever hypersensitivity reaction to just the tuberculo
protein thrown of fin even a dormant tubercular infection could also
occur in any tissue in the body, including the brain, in infants already
hyper sensitized to tuberculous protein while in their mother's womb.
Burnand Finley showed damage and death of cells as well as acute
inflammation in the meninges in such instances [84].
The inflammation that resulted required no TB bacilli, just the
sustained diffusion of the protein of the tuberculosis bacilli or its
active split products through the placenta into a previously sensitized
infant.
Through it all, one thing was certain: Tuberculosis
did not always kill. That infants could survive even a massive dose of
tuberculosis was amply demonstrated in the tragedy called the Lubeck
episode [85].
In the German city of Lubeck, of 251 infants mistakenly injected with
large numbers of virulent human tubercular bacilli, in correctly thought
to be the TB vaccination called BCG, 71.3 percent survived.
But the number of possible complications in those
infants and children who survived TB's on slaught, including those to
the brain and nervous system, Rich knew, would be enough to keep
symptom-based psychiatry perturb bed and under siege for some time to
come.
University of Pennsylvania Department Of Psychology, 1949
But psychiatry was already under siege. In 1949,
psychologist Philip Ash, in a University of Pennsylvania post doctoral
dissertation, proved that three psychiatrists faced with a single
patient and given identical information at the same moment in time were
able to reach the same diagnostic conclusion only about 20 percent of
the time [86].
Subsequently, Aaron T. Beck, one of the founders of
cognitive-behavioral therapy, published a similar study in 1962, which,
although it found psychiatric agreement a bit higher, at between 32
percent and 42 percent, still left doubts regarding the reliability of a
psychiatric diagnosis in general [87].
Added to this came the Rosenhan experiment, a
well-known probe into the validity of psychiatric diagnosis conducted by
Stanford University psychologist David Rosenhan [88].
Published in Science and entitled "On Being Sane in Insane Places,”
Rosenhan's study consisted of two parts. The first involved the use of
mentally healthy associates or fake patients, who briefly pretended
auditory hallucinations in an attempt to gain admission to twelve
different psychiatric hospitals in five different US states. All of
these mentally healthy persons were admitted and diagnosed with
psychiatric disorders. All were also forced to admit they had mental
illness and to take antipsychotic drugs as a condition for their
release.
Figure 13
The second part of Rosenhan's experiment involved asking staff at a
psychiatric hospital to detect fake patients in a group of people who
were all mentally ill. No fake patients were sent to various psychiatric
institutions in this phase of the Rosenhan experiment, yet staffs at
these institutions falsely identified large numbers of actual mental
patients as pretenders.
The study was considered an important and influential
criticism of psychiatric diagnosis. Rosenhan concluded, "It is
clear that we cannot distinguish the sane from the insane in
psychiatric hospitals.” The study also illustrated the dangers of
depersonalization and theme re-slapping on of a label that goes
on in these institutions.
As a result of such intrusions, the American
Psychiatric Association (APA) in 1973 asked psychiatrist Robert Spitzer
to chair a classification task force to establish more precise medically
oriented parameters. The problem was that such a classification would
still be symptom or syndrome focused. The end result was a
classification manual, along the lines of Emil Kraepelin's rejuvenated
categorizing, entitled the Diagnostic and Statistical Manual of Mental
Disorders (DSM), Third Edition, or DSM- III [89].
Though DSM-III was indeed more reliable than its predecessors, it still
offered no clear definition of the cause of the many different "mental
illnesses” it defined [90].
Without causes, the mere categorizing of psychiatric diseases did not
mean that they were valid to begin with and not the result of direct
physical illness. While the APA admitted it had no idea of what caused
its manual's supposed "mental” illnesses; at the same time, it felt
completely confident in its ability to diagnose and "treat” them.
Paul McHugh, former chair of psychiatry at Johns
Hopkins, noticed that the DSM has "permitted groups of "experts” with a
bias to propose the existence of conditions without anything more than a
definition and a check list of symptoms." This is just how witches used
to be identified.”[91] he noted.
Johns Hopkins Department of Pathology, 1949
Rich knew of numerous cases in which the human
placenta was infected in tuberculous mothers and readily admitted that
infection could easily pass from mother to fetus. But it was in the
frequency that he could find the disease reaching fetal tissue, limited
by the diagnostic capabilities of his time that Rich would have to speak
of TB's transfer from the placenta to the fetus as "rare.” William
Henry Welch, who besides being a pathologist like Rich was also a
bacteriologist, never would have agreed.
Welch was already on record that the mere in ability
to pick up TB in the fetus or newborn wasn't an argument against
frequent transmission to them [92].
There were just too many factors involved, such as the hostile,
low-oxygen environment of fetal blood, which could tame even the most
virulent TB bacilli into dormant forms for some time, making diagnosis
difficult to impossible.
It wasn't only Welch who Rich put himself at odds
with German investigator Baumgarten saw infection of the fetus by the
spores of TB coming from the maternal placenta as a common occurrence [93].
In fact, to Baum gar ten, who held's way over European thinking for
some time, all tuberculosis, including neuro tuberculosis, was most
commonly acquired in the womb, in utero, in most cases-though there
remained the possibility that it could occur through infected sperm-all
be it a much less significant possibility.
Ophuls mentioned that it was a well-established fact
that the semen of tuberculous men contains tubercle bacilli, even in the
absence of genital TB [94].
It was obvious, then, that the ovum from which the fetus will develop
could also become infected. Kobrinsky cites Sitzenfrey as having
"demonstrated the presence of bacilli in the interior of the ovum while
still within the Graafian follicle.” [79]
Friedmann, carefully studying the possibility in rabbits, concluded:
"It should be regarded as proved that tubercle bacilli can enter the
fertilized egg-cell, that the latter does not perish as a result of the
invasion, but may develop into a well-formed animal. In addition, the
bacilli transmitted in this way may still be present in certain organs
of the newborn” [95] and among these organs were obviously the brain and the central nervous system.
That tuberculosis is a sexually transmitted disease
is a certainty. By 1972, Rolland wrote Genital Tuberculosis: A Forgotten
Disease? [96]
And in 1979, Gondzik and Jasiewicz showed that, even in the laboratory,
genitally infected tubercular male guinea pigs could infect healthy
females through their semen by a ratio of one in six or 17 percent [97].
This prompted Gondzik to warn his patients that not only was
tuberculosis a sexually transmitted disease but also the necessity of
the application of suitable contraceptives, such as condoms, to avoid
it. Gondzik and Jasiewicz's statistics are chilling, their findings
significant. Even at syphilis's most infectious stage, successful
transmission in humans was possible in only 30 percent of contacts.
Since Gondzik, many other investigators have confirmed the potential for
TB's sexual genito-urinary transmission.
On the other hand, Schmorl's work supported
Baumgarten's and Welch's contention of routine tubercular transmission
to the fetus through the placenta. Schmorl's work again showed that,
indeed, tuberculous infection of the placenta in tuberculous mothers was
much more common than for merely believed [98].
But perhaps all of this work was up staged by Leon Charles Albert Calmette at the Institut Pasteur.
Institute Pasteur, Paris, France, February 1933
Figure 14
Calmette was on to something. He had confirmed that TB's attack form
going through the virtual filters of the placenta into fetal blood were
viral, filter-passing forms of tuberculosis. Such forms were not being
picked up by Rich's traditional TB stains or cultures. Nevertheless,
they were responsible for wasting and death, even while traversing a
perfectly normal placenta [99,100].
In going against the grain of scientific research
such as that done by Pasteur's Leon Charles Albert Calmette, Johns
Hopkins Rich, for all his authority and stature regarding the
pathogenesis of tuberculosis, was skating on thin ice. Since its
founding on June 4, 1887, the Institute Pasteur, for over a century, was
be a confer research. HIV, tuberculosis, polio, and the plague had all
been probed. In addition, since 1908, eight Pasteur scientists had
received the Nobel Prize for medicine. It was while working at Pasteur
that Calmette developed the world's first-and, to this day,
only-recognized vaccine for tuberculosis, the BCG. He was a force to be
reckoned with[101].
Calmette was fully aware of the void that Robert
Koch, the discoverer of tuberculosis, had left for future scientists
such as Arnold Rich. Koch had done it on purpose. A confirmed
monomorphist, Koch insisted that the TB bacilli had only one form that
caused disease. Extremely influential, Koch moved to make certain that
his operatives kept this view as the one most scientists to this day
have adapted.
Figure 15
Koch knew better. Bacteria and myco bacteria certainly could have more
than one form. With Arm Quist, Koch had observed different forms of
typhoid in the blood of its victims. Nevertheless, Koch would now begin
an intensive campaign to seize and rule the scientific and lay mind that
"legitimate” tuberculosis only assumed one form. Thus,
Brock points out that, despite the fact that Koch was a first- rate
researcher, a keen observer, and an in genious technical innovator, he
went from an "eager amateur” country doctor to "an imperious and author
it areas father figure whose influence on bacteriology and medicine was
so strong as to bed own right dangerous”[101].
And nowhere, according to Brock, was Koch a more dangerous and
"opinionated tyrant” than in his rigid insistence on monomorphism, the
idea that microbes could assume one truly infectious form and one form
only. Yet Klebs, who personally examined Koch's own tubercular cultures,
wrote otherwise [102].
In addition to the traditional rods of TB in Koch's culture plates,
spherical forms were regularly found, as well as branching, slender
filamentous, and granular forms. Many of these could pass a filter and
therefore could be interpreted as being 'filter able viruses'. But all
of them could revert back and become classical tuberculosis.
Koch's one-form rigidity wasn't making him friends.
There was wide spread opposition from those who sensed his lack of
evidence. They gravitated toward the more realistic, better- documented
theories of Nageli and Maxvon Petten kofer, which showed that bacteria
change forms as they evolve. Nageli and vonPetten kofer's views retained
wide support almost to the turn of the twentieth century. Koch
reflexively opposed Nageli's ideas as soon as he heard them. Much of
Koch's clash with Louis Pasteur was also based on Pasteur's discovery of
variability among microbes. In that's cuffle, mentions Brock, Koch
could at times be so personally vicious as to be shocking.
Vicious or not, by 1939, bacteriologists Vera and
Rettgerof Yale openly contradicted Koch. Vera: "The single point on
which all investigators have agreed is that the Koch bacillus does not
always manifest itself in the classical rod shape. While at times and
most commonly the organism appears as a granular rod, coccoid bodies,
filaments and clubs are not rare” [103].
To marginalize such thought, Koch and his followers,
to this day, have banished all forms, except one, into the waste basket
hinter land of "involutional” or "degenerative” forms of tuberculosis
and the mycobacteria. Forms other than TB's classic rod shape didn't
count-no matter how many studies showed that all of these forms could
regenerate to the classical TB rod, Koch and his minions thus somehow
prevailed. To Brock, Koch and his cohorts, up to today, represent a
prime instance of the excessive influence of a "cult of personality.”
The problem was that someone somewhere down the line would have to pay
for such cult-generated ignorance.
Let it be said to their credit that, from the onset,
the French saw right through Koch. Tuberculosis had many forms,
including a filterable viral-like stage in its growth cycle. Although
Fontes was the first to document these, MacJunkin, Calmette, and others
soon followed [104,105].
Again and again, either cultures or extracts of organs from tuberculous
victims, after thorough filtration through Chamber lain L2 filters,
produced tuberculosis when injected into experimental animals. And,
importantly, such forms passed right through the placenta from mother to
fetus. In Calmette's eyes, Koch's own postulates were proving him
wrong.
Some animals injected with viral, filter-passing TB
appeared normal during the time of observation, but when tested with
tuberculin showed positive tuberculin skin tests beginning approximately
twenty-five days after being injected with tubercular tissue or
microbes. Other animals lost weight rapidly And some died of a rapid
progressive infection. It all depended upon the virulence of the strain
of filterable TB being used [106].
In a series of twenty-one infants born to tuberculous women, Calmette,
along with Valtis and Lacomme, concluded that their observations proved
the frequent transmission of tuberculosis from the mother to the fetus
by means of filterable forms of tuberculosis. At the same time, Calmette
established that such viral forms of tuberculosis were in the spinal
fluid of perinatal meningitis [99].
It would take time until main stream microbiology
would be forced to even acknowledge such viral forms. It would take a
Nobel nominee by the name of Lida Holmes Matt man.
Pathology Lab of Arnoldrich, Johns Hopkins, Baltimore, 1950
A struggle was going inside the mind of Arnold Rich,
and its implications would affect Western medicine for decades to come.
Under variations in the forms TB can assume, Rich's words don't always
match his conclusions. He conceded that depending upon the type of
culture plate that tuberculosis is incubated on, the shape of the
organism changes, partly because of the culture medium and partly
because of the age of the culture itself. Even the conditions under
which this growth occurred, such as temperature and amount of oxygen,
figured in. He emphasized that non-acid fast staining rods may be
present, especially in young cultures, where as in older cultures and
infected tissues, "beaded forms” were common. Koch also had noticed
these beaded forms. Somewhat granular and protruding from stalks, Koch
thought they were potential "spores” through which infection could be
propagated. But Koch was unable to observe the granules break off into
separate segments.
Hans Much, on the other hand, for decades, not only
watched the granules break off (Much's granules) but regenerate into
classical TB bacilli [107].
Much was also able to document that the granules weren't always
"acid-fast” when stained, a hall mark for classical TB which resisted
de-colorization by acids during staining. Perhaps this was why Much's
granules were not recognized as the spores of tuberculosis that would,
with time, again become the acid-fast staining TB bacilli
microbiologists looked for.
Then there was M.C. Kahn's work. Kahn, using ideal
technique, described, in the most precise manner, his direct
observations of the growth of minute filter-passing granular forms of TB
into fully developed and virulent bacilli, capable of independent
proliferation and producing progressive tuberculosis [108].
Whether granular or otherwise, such viral-like or
cell- wall-deficient (CWD) forms of tuberculosis, often mistaken for
mycoplasma, are today widely known as "L-forms, "named after the Lister
Institute by one of its scientists, Emmy Kliene Berger [109].
L-forms are cell-wall-deficient by virtue of a breech in their cell
wall that allows them the plasticity to assume other forms, including
granular forms. Little recognized in Rich's time, L-forms of
tuberculosis have since even been found in breast milk [110].
Rich, working in the 1940s, wanted to believe very
much in these viral forms of tuberculosis. They explained the many times
that he knew he was dealing with tuberculosis but could not, even as a
pathologist, see the germ. Nevertheless, this knowledge, relatively new
at the time, was not substantiated enough. After all, Kahn had observed
the transformation of granular forms to mature bacilli in vitro in a
culture plate. This did not mean to Rich that every TB bacilli once in
humans had to go through this same cycle in its reproduction. So,
despite Kahn directly assuring him by personal communique that he had
solidified his findings in vivo in laboratory animals, Rich was not
ready to acknowledge granular viral cell-deficient forms of
tuberculosis, which were key to the mystery of how certain forms of TB
sieved through the placenta's chorionic villi into the fetus, escaping
detection.
Rich's statement that, in certain cases, even when
the maternal placenta was laced with TB bacilli, "acid-fast stains of a
large number of sections of the fetal tissues failed to disclose a
single bacillus” was correct. Welch had predicted it. The viral
cell-wall-deficient (CWD) forms could only be picked up by special
stains, cultures, and techniques that Rich had no access to.
In the mean time, Rich's hypothetical statement of
"rare” transmission was having difficulty. Many infants were reacting to
the TB skin test weeks to months after birth, even without known
exposure after birth.
Department of Biological Sciences, Wayne State University, Detroit, Michigan, 1982
Lida Holmes Mattman, PhD, had an impressive and well-
rounded back ground. Having earned an MS in virology from the
University of Kansas and a PhD in immunology from Yale University,
Mattman taught immunology, microbiology, bacteriology, virology, and
pathology. She worked for thirty- five years at institutions such as
Harvard, the Howard Hughes Institute, Oakland University, and Wayne
State University. As both a virologist and a bacteriologist, Mattman was
equally at home developing the first complement fixation with bacteria-
free virus and doing extensive work on various bacteria. And the fact
that she was a virologist added all them orecredencetoherin-
depthstudiesrelatedtoviral-likebacterialL-forms (also called Cell-Wall-
Deficientor CWD forms). So unique were her findings that in 1998 Mattman
was nominated for the Nobel Prize in medicine. In 2005 she was inducted
into the Michigan Women's Hall of Fame.
Figure 16
Mattman authored the book Cell Wall Deficient Forms: Stealth Pathogens,
now in its third edition. The book is described as follows: Numerous
infectious diseases are described as idiopathic, meaning that "the cause
is a complete mystery.” For many idiopathic diseases, the causes become
clear when certain techniques are applied to the patient's blood or
other tissues. Cell Wall Deficient Forms: Stealth Pathogens, Third
Edition describes these techniques. In the case of tuberculosis, a
disease that has recently regained importance because the strains have
acquired antibiotic resistance, the book describes a method that is
widely used a broad. This method typically renders the diagnosis within
72 hours.
If the answer to unraveling the mechanism behind
autism was an infectious one, Lida Holmes Mattman was who you would want
to have investigating it.
Microbiologist and virologist Mattman knew something
that few scientists on the planets till truly understand. Bacteria have a
lifecycle and can assume many forms. She also knew which special
stains, cultures, and techniques would have to be used for the best
chance to detect them. Mattman, of course, had access to modern
techniques that her predecessors didn't, including electron microscopy,
immune fluorescence, polymerase chain reaction (PCR), and other
molecular assessment techniques. These helped, but in the case of
tuberculosis, especially cell- wall-deficient tuberculosis, they did not
always work. She first wrote Cell Wall Deficient Forms in 1974 [111].
Instantly, it was held in high regard. The problem was that, at that
point, not all microbiologists were accepting it. By 2001, Mattman had
concluded, regarding the human placenta, that: "There is little doubt
that the minute filterable form of bacteria move from the mother's
capillaries to those of the fetus.” She was referring, of course, to
tiny filterable bacteria either without a cell wall or those having a
breach in that cell wall. Mattman was an expert on such forms, and as
her book went into its third edition in 2001, she also referred to them
as "stealth pathogens,” which went beneath the radar of modern
laboratory diagnostics [112].
Once a pathogen like tuberculosis had its cell wall disrupted, it
become plastic, having the ability to assume many forms. Some were so
tiny that they passed through a 22|im filter, the so-called viral stage
of a bacteria. Cell wall disruptional so changed the way these microbes
stained. Cell-wall-deficient tuberculosis did not stain with the same
acid- fast stain that classical TB bacilli did.
Actually tuberculosis was one of the first placental
infections to be accurately described. Since Lehmann's first report, the
subject had come under intense scrutiny. Mattman spent considerable
time talking about the trans placental passage of cell-wall-deficient
forms of TB to the fetus. She knew that fall the pathogens, tuberculosis
and its related mycobacteria relied on their stealth,
cell-wall-deficient forms, many of them both dormant and resistant, for
their singular survival record inside humans. Thus, she was drawn, early
on, to the subject. Her 1970 article remains a classic on such
tubercular forms [113].
Calmette, said Mattman, knew that TB must traverse the placenta in its
viral stage since the placenta, in most cases, remained intact with no
obvious damage. Calmette noted that after such infection with
cell-wall-deficient tuberculosis, quick fetal death might occur. Even if
the child were born alive, it could result in death through hemaciation
with in one month. Yet there were cases in which the infant suffered no
ill effects [114].
These were the infants who were infected but nevertheless vigorous for
the time being-until the stealth forms of their dormant tuberculosis
could spring back to their classical virulent forms. This dove tails
with Kanner's thirty-months-after-birth allowance for the onset of
autism (Figure 17).

What really troubled Lida Mattman were those cases,
established in the early 1970s, in which seemingly healthy mothers, with
no symptoms, were able to pass to their infants cell-wall-deficient
forms of TB which nevertheless killed or infected their off spring. So
stealth was cell-wall-deficient tuberculos is in the menstrual blood
from one mother whose off spring became ill a few days after birth that
it took eight animal passages to finally yield the tubercular pathogen [115].
Mattman warned that tuberculosis mainly grew as pleomorphic (many-formed) stealth pathogens [116].
In one long series, US labs were only picking up 50 percent of
tubercular sputum samples by not using special cultures for its
cell-wall- deficient forms [117]. Mattman didn't assume that these labs’ ability to pick it up in the blood or cerebro spinal fluid would be much better
Brieger, working at Cambridge University,
demonstrated mainly pleomorphic stealth growth when he inoculated
tuberculosis directly into the amnioticsac of lab animals [118].
The outer layer of the amnioticsac is part of the placenta. Rapidly,
cell-wall-deficient granules formed that did not stain with traditional
acid- fast stain. Within three days, other cell-wall- deficient forms
such as the long branching fungal filaments of TB appeared. TB is a
mycobacteria with both bacterial and fungal (my come an s fungal) forms.
Brieger repeated the study using fowl tuberculosis in chicken embryos.
His results were similar [119]. Cell-wall-deficient forms formed, again not identifiable by traditional stains or cultures.
Dorozhkova spoke about congenital trans-placental tuberculosis from mother to fetus [120].
And by 1996, Insanov warned that an infection transmitted this way with
cell-wall- deficient forms of TB in children not only made standard
treatment less effective but created a disease with a gradual, insidious
onset and a slow accumulation of cerebral damage in children [121].
This made the disease more difficult to diagnose, because its slow burn
into young nervous systems allowed months to years before its full
spectrum of damage was obvious. Insanov showed that cell-wall-deficient
forms in tuberculosis meningitis accounted for an incredible 87.6
percent of the tuberculosis found in children with TB meningitis and
87.3 percent of those in adults. How could such statistics be ignored?
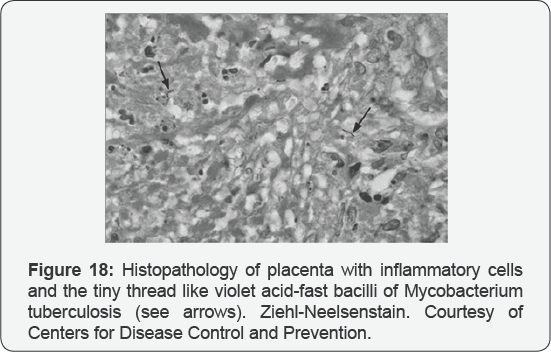
Figure 18
It's not that Americans hesitated to acknowledge the importance of
latent or dormant tuberculosis and how it could persist within a child
or adult for years without causing disease [122]. They just couldn't seem to correlate the phenomena with Mattman's stealth pathogens.
To Lida Holmes Mattman, it was bad enough that most
twenty-first-century bacteriologists still ignored those cell-wall-
deficient bacterial forms responsible for much adult illness of
"unknown” cause. But with such stubbornness, perhaps, there was a just
retribution involved in that the same researchers who ignored her
findings were suffering along with the general population. But when it
came to innocent children and newborns not being diagnosed or treated
properly for disease because of such stubborn recalcitrance-she could
simply not accept this.
Conclusion
The consensus that autism is caused by intra uterine
infection has been growing. In a 2007 issue of Science, Patterson
hypothesized that by far the most important environmental risks for
autism and schizophrenia consist of intra uterine infection before birth
[123].
Fatemi, in 2009, mentions the same: that based on major agreement and
several decades of studies, maternal infection is responsible, leading
toward autism and schizophrenia [3].
The evidence for mental illness, including autism and schizophrenia,
being the result of an infectious disease is quite extensive.
Medical residents are often told, "Don't look for
zebras. Don't look for the exotic or the esoteric cause of a disease.”
And the best diagnosticians follow this advice. For the purposes of this
document, part of not looking for zebras includes asking what
infectious process statistically most affects not only women of child
bearing age but their children-and at the same time is nerve-seeking
(neurotropic) and fully capable of delivering the myriad symptoms now
acknowledged to be the autistic spectrum. According to statistics such
as those that can be obtained from the World Health Organization and a
host of other sources, that disease, hands down, is tuberculosis and its
related mycobacteria.
Just as appropriate, were this the case, might be the
admonishment of a resident who brings up the issue of vaccines or their
ingredients as a direct (as opposed to an indirect) influence on
autism. One must always distinguish primary cause from aggravating
circumstance. First, most of the vaccines in today's infant/ maternal
schedules have a direct contraindication to such potential chronic, even
dormant, tubercular infection. And on top of this, physician and
researcher Hartz, after sizable human trials, published an article in
the Journal of the American Medical Association insisting that mercury
compounds were "positively injurious and detrimental to one afflicted
with tuberculosis.” [4].
If this is so, then it easily follows that a mercury-bearing substance
like the merosal would only worsen an existing infection.
In addition, some of the oil adjuvants used to
increase a vaccine's potency are lipids or oils that are cholesterol
precursors, becoming cholesterol in the body [124].
Such a cholesterol surgeries a big boost for any dormant systemic
tuberculosis already in the body, whose very ability to maintain
infection is linked to its ability to acquire and utilize cholesterol.
So crucial is this unique ability of TB to use cholesterol in the body
for both carbon and energy sources that if it were not for its ability
to grow off cholesterol, tuberculosis, unlike other pathogens, would be
unable to resist eradication through cytokine attack and the attempts of
certain activated white blood cells called macrophages to starve it of
essential nutrients. Cholesterol utilization is one of many true
survival mechanisms acquired after ones, which has made TB, from a
historic sense, probably the most successful human pathogen on the
planet [125].
So in comparative and simpler terms, one might look
at an injection of certain vaccine adjuvants, squalene among them,
whether inside or outside of a vaccination, a slighting up chronic foci
of tuberculosis like a Christmas tree. This does not mean that
vaccinations or mercury perse cause autism, although certainly either is
capable of precipitating a child's original autistic event by acting in
synergy with the infection behind autism. Thus, they could very well
appear to be its cause. J.Langdon Down, who was the first to deal with
autism in his own children, thought that autism, "for the most part,”
originated from TB in children's parents. He was also the first to use
the term developmentally disabled for such cases, a euphemism that the
public liked and could much more readily handle than the develop
mentally disabled from tuberculosis. Was John Langdon Down just pulling
from an imaginary short list when he focused on the fact that, in most
cases, his develop mentally disabled children, including those with
autism, resulted from parental tuberculosis? Not-at- all. Down was a
high-end product of English science, and what the British lacked in the
well-organized and well-financed state- run laboratories of the Germans,
they more than made up for in their astute powers of observation. Down
was skilled at autopsy, and his studies' results came directly with how
many times he found the disease in his children. Down also could, even
then, draw on an extensive library of research on the subject which
pointed toward the same direction as his thoughts. It was only then, and
after compiling compelling statistical evidence, that he came to the
conclusion he came to and published his thoughts.
With time, more evidence accrued. Antidepressants,
hailed as new breakthrough drugs in the mentally ill, were really
discovered as a by-product of the tuberculosis research of the 1950s.
Having proven anti-tuberculous activity, they weren't used clinically as
anti-depressants until the 1960s. The first was imipramine, now called
atricyclic antidepressant. Almost concomitantly came antidepressants
known as Mono-Amine- Oxidase (MAO) inhibitors, also with anti-tubercular
activity. This was only after it was noted that TB patients given MAO
inhibitors experienced a state of elation and euphoria where only
depression had existed before. No wonder. MAO inhibitions had activity
against their infectious disease. Yet from their onset, results and
studies, no matter how much they confirmed TB's role in mental illness,
were tainted by a public that wanted to hear none of them. After all, to
be diagnosed in sane or develop mentally disabled and tubercular at the
sametime were two of the greatest stigmas that could be thrust up on a
patient and his or her immediate family. So in sanity or mental illness
was either given medical labels that few understood or reduced to a
"nervous disorder” with TB always that "not me” illness. Rather it was
often referred to as a "chest ailment” during which "nervous disorders”
often occurred.
In 1997, Adhikari, Pillay, and Pillay were quite
straight forward on a subject traditionalists never have admitted to as
other than "a rarity” [126].
They wrote in "Tuberculosis in the Newborn: An Emerging Problem”:
Congenital TB can result from hematogenous (blood) dissemination of
M.tuberculosis after maternal mycobacteremia, rupture of a placental
tubercle into the fetal circulation, or ingestion of infected amniotic
fluid or maternal blood at delivery. The mother might not have symptoms
of TB disease, and subclinical maternal genital TB also can result in an
infected neonate. This seems straight forward enough. The fetus can be
infected by the mother with TB while still in her womb. The mother might
not have symptoms of TB. And it was an "emerging problem.” But another
emerging problem was happening at about the same time. Autism had begun
to sky rocket.
The extent of the diagnostic problem involved in
finding cerebral tuberculosis in infants is documented by Rock et.al. in
an April 2008 issue of Clinical Microbiology Reviews. In this Rock
mentions that some pediatric experts recommend that all children under
12 months of age should have a lumbar puncture due to both their
susceptibility to cerebral tuberculosis and the difficulty in clinically
evaluating infants with it [127].
Most will not entertain this, but it does emphasize the extreme
difficulty in diagnosing the disease in infants. Similarly, by 1999,
Pillet, in an article in the Archives of Pediatrics, went over the
difficulties in early diagnosis of neonatal tuberculosis. His
conclusion, and the conclusion of so many others before him, was that
its frequency was being under estimated and its diagnosis often
difficult because its initial manifestations were often delayed
[128]
. By stating this, Pillet was saying what Insanov, Calmette and Welch
had already brought up regarding the distinct delay of disease process
as a result of the cell-wall-deficient forms of tuberculosis in the new
born which would take time to revert to classical disease. This is also
what Mattman brought attention to. Calmette warned pathologists that CWD
forms caused few tissue changes to the placenta, and Mattman warned
that even healthy, otherwise a symptomatic pregnant women with a focus
of tuberculosis somewhere in their body could generate stealth,
cell-wall-deficient forms of tuberculosis into the blood to infect their
fetuses. Rich had already pointed out the extreme activation of even
silent TB that occurs during pregnancy, a fact he had acquired from
Norris before him [78].
In October 2003, Gourion and Pelis solo reported in
the Journal of Autism and Developmentalv Disorders on how neonatal
cerebral tuberculosis had evolved into a member of the autistic spectrum
of disorders, namely Asperger's syndrome
[129] .
More importantly, Gourion mentions that
across-comparison between neuropathology and imaging studies done on TB
meningo encephalitis and those from the autistic spectrum, including
Asperger's seemed to match, including a study of the decreased
metabolism in the brain's cingulated gyri [130-135].
This was important. In linking Asperger's syndrome, a known disease in
the autistic spectrum to neonatal TB meningitis Gourion and his
colleagues Pelis solo, Orain-Pelis solo and Lepine joined Schoeman's
previous implication that tuberculosis and its neonatal brain lesions
were behind the neuro developmental disorders,including the autistic
spectrumofin fancy,childhood,andbeyond [135].
No one who has ever witnessed the pathetic head
banging of an autistic child can truly come away un swayed. Many
explanations have been offered by workers in the field, some of them
unconvincing. That pain relief is a possibility has occurred to a few.
They mention a child is more likely, for example, to bang his or her
head when the child has a near infection or is suffering from some other
physical discomfort in the head. This makes sense, but some of the
other explanations do not. Five out of 11 of Kanner's initial subjects,
through measurement, "had relatively large heads”, which could indicate
possible degrees of hydrocephalus. Delacato, evaluating 474 children
diagnosed as autistic found 81 percent of these to have enlarged
ventricles on computerized tomography, a premier radiologic feature of
hydrocephalus [136].
Edwards and many others have documented the chronic head-aches that can
result from hydrocephalus, one of whose more frequent causes in infants
is perinatal infection [137,138].
In fact hydrocephalus itself is often listed as a possible cause for
autism. As previously mentioned, at one time, the diagnosis of acute
hydrocephalus was so commonly associated with cerebral tuberculosis that
the terms were used interchangeably
It is for all of these considerations, as well as for
the sake of the developmentally disabled and autistic children in our
midst today, no less those that will grow to adolescence and adulthood,
that we carefully review the historic and present debate of
tuberculosis's stealth role in the psychiatrically impaired and those
children that are developmentally disabled or autistic.


Comments
Post a Comment