Attention-Deficit Hyperactivity Disorder-Juniper Publishers
Global Journal of Intellectual & Developmental Disabilities (GJIDD)
ADHD is the most common neuro-behavioral disorder of
the child. The present review article summarizes various aspects of its
etiology, symptomatology, diagnostic methods, and various aspects of
management. The disease need to be treated by a inter-disciplinary team
including pediatricians, psychologists, sociologists etc and there is
need to involve parents, school staff and if possible the children
himself and must be based around the establishment of good working
relationships with family and school.
Introduction
Attention-deficit/hyperactivity disorder (ADHD), a
multi-dimensional syndrome is the most common behavioural disorder of
children [1],
characterized by symptoms of inattention, impulsive behaviour and
hyperactivity resulting in behavioral problems and poor academic
performance. The hallmark of ADHD is problem of sustaining inhibition (a
mental process that restrains an action, behaviour or emotion) rather
than sustaining attention.
Prevalence and Epidemiology of ADHD
Prevalence of ADHD among school-aged children in different studies varies between 5-12% [2,3], and the disorder is reported to decline with increasing age [4].
Boys are 2.4-4 times more likely to have the illness than girls. The
disorder is found in all cultures, and is known to persist into
adulthood. The overall prevalence in adults is about 4.4%. About 35 -65%
of ADHD children will continue to have the disorder in adulthood [5]. Of these, 15% will show no improvement in adult life, while the remainder will experience partial improvement [6].
Etiology and Risk Factors
The exact cause of ADHD is still an enigma. Many
theories have been put forward to explain the syndrome viz. chemical
(neurotransmitter) theory, frontal lobe disorder theory, genetic theory,
environmental factors etc.
Chemical (Neurotransmitter theory)
Neurotransmitters (Nor epinephrine and dopamine) are
used by the brain to stimulate or repress stimulation in brain cells. To
pay proper attention, the brain must be adequately stimulated. To have
proper control of our impulses, areas of the brain must be adequately
controlled, repressed, or slowed down. In ADHD children, both systems of
stimulation and repression are not working correctly. Some studies
suggest that ADHD Children/Adults may have only ten to twenty-five
percent of these two neurotransmitters found in the normal brain [7].
Frontal lobe disorder
Frontal lobe of brain is destined with planning and
organizing different tasks. It controls many aspects of everyday life.
This part of brain is involved in decision making, planning, error
detection, resisting temptations and impulse control-these functions are
also known as "executive functions”. It has been observed that in
children with ADHD, these “executive” areas of the brain are
under-active. Moreover increasing activity in this area has been shown
to decrease behavioural symptoms. A decreased frontal lobe mass has also
been reported in these children [8-10].
Genetic
Since the disease is said to run in families, genetic
factors are sure to be blamed. Genetic variation in dopamine receptor
genes DRD4 and DRD5, have been consistently associated with ADHD [11].
Other genes were also linked to ADHD, such as the Dopamine Beta
Hydroxylase gene (DBH), the glutamate receptor gene (GRM7), the
serotonin transporter gene (5HTT), and the serotonin receptor 1B gene
(HTR1B) [12].
Environemental factors
Role of environmental factors is uncertain; they may
influence symptoms of ADHD (sub-syndromic) rather than the syndrome of
ADHD [13].
Most of these factors, which are associated with ADHD, are pregnancy
and birth related risk factors which are classified into three groups
including prenatal, perinatal, and postnatal risk factors.
Prenatal risk factors
A large number of studies have shown that maternal
exposure to alcohol, tobacco, and cocaine during pregnancy increases the
risk of ADHD. Various studies have demonstrated that preeclampsia,
maternal anemia, lower serum level of iron and iodine, and trauma to
abdomen during pregnancy are associated with increased risk of ADHD
development [14,15].
Perinatal risk factors
A number of risk factors such as prematurity, low
birth weight and breech delivery have shown consistent association with
increased risk of ADHD [16].
Postnatal risk factors
Postnatal viral infections such as measles,
varicella, and rubella increase the risk of developing ADHD.
Additionally, several other factors such as breast-feeding, head injury
in early childhood and adolescence, encephalitis, convulsion and
endocrine disorder are estimated to be risk factors for development of
ADHD [12]. Incidence of ADHD has been shown to be more common in children with lower rates of breast feeding [17].
Other factors
It has been observed that adverse family environment
variables such as family conflict, decreased family cohesion, and
exposure to maternal psychopathology, low social class, large family
size, foster care placement increases the risk for developing ADHD [14].
Iron and zinc deficiency has also been implicated in ADHD, which is
notable because both are required for the production of Nor Epinephrine
and Dopamine [18].
Symptoms and Diagnosis
The diagnosis of ADHD is made by careful clinical
history. Many-a-times it is difficult to differentiate between a normal
and ADHD child. Since ADHD is a behavioural disorder hence there are
hardly any positive physical findings. Similarly no laboratory
investigation is available to confirm the diagnosis. Onset is usually
before seven yrs of age. The child has an entirely different behaviour
not primarily attributable to poor parenting, lack of discipline, low
motivation etc. The abnormal behaviour is observed at several
settings/situations. The features persist over time. The disturbance
causes clinically significant distress or impairment in social,
academic, or occupational functioning. Before labeling ADHD problems
like sleep disorders, anxiety, depression, and certain types of learning
disabilities must be excluded. Children with ADHD and with clinical
features of autism should also receive genetic testing to rule out
Fragile X syndrome [13]. It has to be kept in mind that every child that fidgets and/or behaves defiantly is not ADHD.
The child often fidgets or squirms about when seated,
shifts rapidly from one task to another without completing first task
or activity, speaks irrelevantly, out of turn or speaks excessively,
does not listen, can engage in dangerous activities causing harm to
himself/herself [7].
The neuro-behavioral disorder is marked by inattention, difficulty in
controlling impulses and excessive motor activity. The child should be
labeled as ADHD only if the symptoms persist for more than six months.
There is no single test to iagnose ADHD, currently, there are two widely
used diagnostic criteria for ADHD: the International Classification of
Diseases (ICD) by WHO and the Diagnostic and Statistical Manual of
Mental Disorders (DSM) by American Psychiatric Association. These scales
include the Conners Index Questionnaire, and the Vanderbilt ADHD
Diagnostic Teacher Rating Scale [13].
ICD- 10 uses the name "hyperactivity disorders” to emphasize the two
major symptoms, attention disorder and hyperactivity (impulsivity),
which occur simultaneously and in multiple occasions such as home and
school. This standard excludes other mental dysfunctions including
anxiety disorder, mood disorder, pervasive developmental disorder and
schizophrenia.
DSM-5 Criteria for ADHD
People with ADHD show a persistent pattern of
inattention and/or hyperactivity-impulsivity that interferes with
functioning or development [19].
Inattention
Six or more symptoms of inattention for children up
to age 16, or five or more for adolescents 17 and older and adults;
symptoms of inattention have been present for at least 6 months, and
they are inappropriate for developmental level:
Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
1. Often has trouble holding attention on tasks or play
activities.
2. Often does not seem to listen when spoken to directly
3. Often does not follow through on instructions and fails
to finish schoolwork, chores, or duties in the workplace (e.g.,
loses focus, side-tracked).
4. Often have trouble organizing tasks and activities.
5. Often avoids, dislikes, or is reluctant to do
tasks that require mental effort over a long period of time (such as
schoolwork or homework).
6. Often loses things necessary for tasks and
activities (e.g. school materials, pencils, books, tools, wallets, keys,
paperwork, eyeglasses, mobile telephones).
7. Is often easily distracted
8. Is often forgetful in daily activities.
Hyperactivity and impulsivity
Six or more symptoms of hyperactivity-impulsivity for
children up to age 16, or five or more for adolescents 17 and older and
adults; symptoms of hyperactivity-impulsivity have been present for at
least 6 months to an extent that is disruptive and inappropriate for the
person's developmental level
Hyperactivity
i. Often fidgets with or taps hands or feet, or squirms in seat.
ii. Often leaves seat in situations when remaining seated is expected.
iii. Often runs about or climbs in situations where
it is not appropriate (adolescents or adults may be limited to feeling
restless).
iv. Often unable to play or take part in leisure activities quietly.
v. Is often "on the go” acting as if "driven by a motor”
vi. Often talks excessively
Impulsivity
i. Often blurts out an answer before a question has been completed.
ii. Often has trouble waiting his/her turn.
iii. Often interrupts or intrudes on others (e.g., butts into conversations or games).
In addition, the following conditions must be met.
i. Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
ii. Several symptoms are present in two or more
setting, (such as at home, school or work; with friends or relatives; in
other activities).
iii. There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
iv. The symptoms are not better explained by another
mental disorder (such as a mood disorder, anxiety disorder,
dissociative disorder, or a personality disorder). The symptoms do not
happen only during the course of schizophrenia or another psychotic
disorder
Changes in the DSM-5
The fifth edition of the DSM was released in May 2013
and replaces the previous version, the text revision of the fourth
edition (DSM-IV-TR). There were some changes in the DSM-5 for the
diagnosis of ADHD.
i. Symptoms can now occur by age 12 rather than by age
6.
ii. Several symptoms now need to be present in more than one setting rather than just some impairment in more than one setting.
iii. New descriptions were added to show what symptoms might look like at older ages.
iv. For adults and adolescents age 17 or older, only 5 symptoms are needed instead of the 6 needed for younger children.
Types of ADHD
Based on the types of symptoms, three kinds (presentations) of ADHD can occur
Combined Presentation (ADHD-C): If enough
symptoms of both criteria inattention and hyperactivity-impulsivity were
present for the past 6 months. CT represents the most common
sub-population of ADHD patients, and has combined higher ODD, CD,
anxiety and depression disorders, leading to social dysfunction and poor
prognosis [20].
Predominantly Inattentive Presentation (ADHD-I):
If enough symptoms of inattention, but not hyperactivity- impulsivity, were present for the past six months.
Predominantly Hyperactive-Impulsive Presentation (ADHD-HI):
If enough symptoms of hyperactivity-impulsivity but not inattention
were present for the past six months. Combined type ADHD had the highest
rates of co-morbidity with oppositional defiant disorder as compared to
the ADHD HI and ADHD-I. Studies have shown that there were poor
academic scores, combined with anxiety and depression in PI type
patients, which mainly consist of girls and adolescents. Children with
HI type generally have no academic problems, but are more likely to be
complicated with conduct disorder.
Comorbidities
It is well established that ADHD frequently is
co-morbid with other psychiatric disorders like oppositional defiant
disorder (ODD), conduct disorder (CD), substance abuse disorder, and
anxiety disorder [20].
Depending on the precise psychometric definition, 25%-35% of patients
with ADHD will have a coexisting learning or language problem [21]. Nearly one- fourth of ADHD children have an associated learning disorder of reading, spelling, writing and arithmetic [18]. ADHD is also associated with academic underachievement and cognitive impairment from pre-school age to adulthood [18].
In addition, children with ADHD have several associated difficulties in
various domains of functioning, including adult relationships (e.g.,
noncompliance with adult requests), school functioning (e.g. classroom
disruption, poor achievement), and peer and sibling relationships (e.g.
annoying, intrusive, overbearing, and aggressive behaviours) [18]. Children with ADHD have higher rates of tic disorders [21],
which may contribute additional dysfunction due to distractions and
social impairments directly attributable to the movements or
vocalizations themselves.
Treatment
Management of ADHD is in fact an art. Patients must
be managed by a team of doctors (pediatricians, psychologists,
sociologists) with full involvement of parents. Both doctors and parents
must understand that it's tough for the individual has to cope with
daily frustrations. It's rough on family members whose lives are
regularly disrupted by the disorganization, outbursts, temper tantrums
or other misbehaviour of the child or teen. It's normal for parents to
feel helpless and confused about the best ways to handle their child in
these situations. Because kids with ADHD do not purposely decide to act
up or not pay attention, traditional discipline-like spanking, yelling
at, or calmly trying to reason with your son or daughter -usually
doesn't work [22]. The Figure 1 depicts the algorithm which can be taken as guidelines by the treating team [13]. Hence, treatment should be under three heads and they can be given alone or in combination
i. Pharmacotherapy
ii. Psycho-therapy or behavioral therapy, and
iii. Educational interventions.
The initial focus of treatment is to reduce the core
symptoms of ADHD. Medication is usually offered as first-line treatment
for patients aged 6 years and over while non-pharmacological treatment,
consisting primarily of parenting interventions that focus on
behavioural management, is generally recommended for children under 6
years of age.
Pharmacotherapy
Psycho-stimulants are the first line drugs and are
highly effective for 75 - 90% of children with ADHD. They consistently
reduce ADHD core features [23].
They have their greatest effects on symptoms of hyperactivity,
impulsivity, and inattention, and the associated defiance and
aggression. They improve classroom performance and behavior and promote
increased interaction. Yet, psycho-stimulants do not appear to change
long-term outcomes such as peer relationships, social or academic
skills, or school achievement [24]. The most common stimulant
medications (amphetamines) are
a. Methylphenidate: MPH
b. MPH Transdermal Patch
c. Dexmethylphenidate
d. Oros-Methylphenidate
e. Dextroamphetamine
f. Pemoline
g. Lis-Dexamfetamine
Nonstimulant therapy: The only approved drug
in this category includes atomoxetine. It is a nonselective
noradrenaline reuptake inhibitor that results in increased synaptic
noradrenaline. Atomoxetine is used in children with a failed stimulant
trial as first line therapy due to untoward side-effects, e.g. mood
fluctuations or tic disorders, or those with a history of substance
abuse [21].
Antidepressant treatment
These drugs are used when drugs described above failed to deliver good results [22].
a. Buproprion hydrochloride-an antidepressant that
is involved in the reuptake inhibition of dopamine and noradrenaline and
potentiates dopaminergic neurotransmission. It decreases hyperactivity,
aggression and conduct problems.
b. Imipramine or nortriptyline-these are tricyclic
antidepressants which can improve hyperactivity and inattentiveness.
They can be especially helpful in children experiencing depression or
anxiety. During overdose, the tricyclic antidepressants have the highest
risk of cardiovascular side-effects. Therefore, they should be the last
line of therapy.
c. Clonidine hydrochloride-used to treat high blood
pressure, clonidine also can help manage ADHD and treat conduct
disorder, sleep disturbances or a tic disorder Research has shown it
decreases hyperactivity, impulsivity and distractibility, and improves
interactions with peers and adults.
d. Guanfacine-this antihypertensive decreases
fidgeting and restlessness and increases attention and a child's ability
to tolerate frustration. Tenex is the short-term preparation, while
Inuniv is the long-term preparation
Duration of treatment: As this disease is a
chronic one lasting for years or for even lifetime, medications are to
be given for a long time. Duration of therapy has to be individualized
and parents must be explained in detail about the adverse effects of the
drug. They must also be warned not to stop the drug without prior
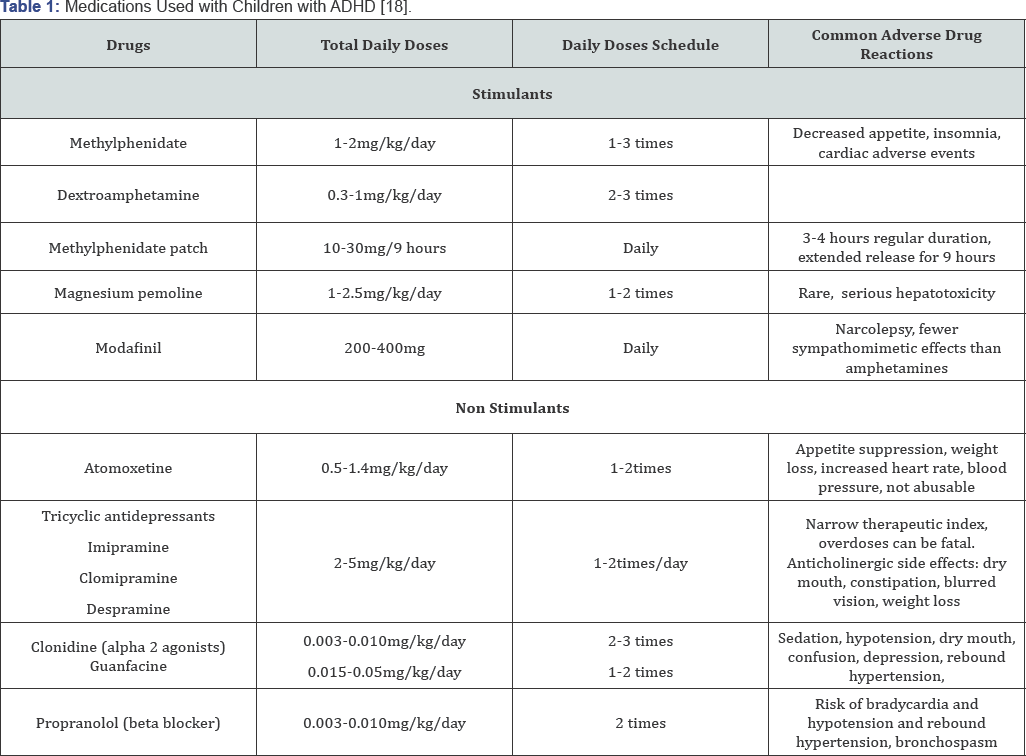
consultation (Table 1).

Behavioral therapy
Behavioural approaches represent a broad set of
specific interventions that have the common goal of modifying the
physical and social environment to alter or change behaviour.
Behavioural therapy is a multi pronged approach including parents as
well as a wide range of professionals, such as psychologists, school
personnel, community mental health therapists, and primary care
physicians and most importantly child himself. The hallmark of therapy
is rewarding approach. The child's behaviour should be studied in detail
and the team should choose a negative behaviour that needs change and a
positive behaviour that should be allowed to continue [25].
For every positive response child should be rewarded, needless to say
the reward must be as per the liking of the child and should be
motivational. The plan designed must be individualized and should be
changed if it fails to deliver. The school teachers and management also
need to be educated about the disease and they should also be taught how
to manage these child. Many a times it is better to form a group of
parents of ADHD children [25]. Behavior therapy is best given by parents [26]. Older siblings can also be involved (Figure 1).
Educational interventions
Many-a-times the normal children may make a joke of
the ADHD children making his treatment more worse. Hence, educational
interventions also have a big role to play. Not only his class-mates be
taken into confidence, there should also be classroom modification,
proper accommodation, special attention from the school staff,
personalized syllabus etc



Comments
Post a Comment