JUNIPER
PUBLISHERS-
Global Journal of Intellectual & Developmental Disabilities (GJIDD)
The symptom of insomnia is one of the most common
complaints among the elderly during their aging process. It is defined
as the subjective reported insufficient quality or quantity of sleep
despite adequate sleeping conditions. The prevalence of insomnia could
reach 40%-50% among the elderly and significantly affect their quality
of life. This paper aims to conduct systematic review on previous
studies to evaluate the effectiveness and summarize the treatment
characteristics of acupressure. Limitations and recommendation were
provided as future directions of therapeutic garments development for
the elderly. This new concept of acupressure therapeutic garment could
help to identify the future development directions of therapeutic
function garments and provide promising methods to improve the insomnia
and life quality of the elderly.
Keywords: Insomnia; Elderly; Therapeutic garment; Acupressure
The aging process is universal and biological that
everyone must experience. Both psychological and physical changes may
occur when people becoming old and the symptom of insomnia is one of the
most common complaints among the elderly [1,2].
Insomnia is defined as the subjective reported insufficient quality or
quantity of sleep despite adequate sleeping conditions [3,4]. Prevalence of this symptom increases along with age resulting that about 40%-50% of the elderly suffering from insomnia [1,5,6].
Insomnia among elderly may have many negative
influences on their general health and life quality. Specifically,
insomnia could cause daytime fatigue and malaise, poor concentration,
memory loss, cognitive decline, mood disturbances, daytime sleepiness or
other symptoms such as headaches, hypertension and gastrointestinal
problems [3,5-8].
Moreover, the statewide research conducted by the Michigan Nursing
Homes indicated that the ignorance of insomnia could highly lead to the
risk of falls (increased by 50%) which may cause a higher rate of
mortality among the elderly [6,9].
However, many people in the public including some doctors have the
misconception that the symptom of insomnia among elderly is normal and
accepted as the process of aging. Actually, the insomnia was caused by
both medical and psychosocial factors as co morbidities [10]. To summarize, the common causes of insomnia among elderly are:
- Physical symptoms, such as chronic low back pain, joint diseases etc.
- Underlying medical condition or side effect of medication.
- Mental diseases, such as anxiety or depression.
- Environmental or behavioral factors. [3,6,11,12].
To treat for the insomnia among elderly, treatments
could be classified into Pharmacological and Nonphamacologic therapy.
Pharmacological treatment includes some drugs such as Benzodiazepine
sedative hypnotics, Non-benzodiazepine sedative hypnotics, Sedative
antidepressants which could make people calm down and feel sleepy. Non
phamacologic therapy refers to Bright light therapy, Cognitive behavior
therapy, Stimulus control therapy, Sleep Hygiene, etc. [3,4,13].
However, although there are numerous normal and
tradition treatments for insomnia, there still remain limitations since
the group of elderly is special. Most of the cases, elderly have a rich
medical history. They not only suffered from the symptom of insomnia but
also have other diseases such as heart diseases and hypertension.
Generally, the health condition of the elderly is weaker than younger
adults. If receiving pharmacological treatment, side effect could be a
big issue especially when there is a drug interaction because many
elderly take other medication for different diseases [14].
Then if non pharmacological treatment adopted, corresponding conditions
including professional devices, room for treatment, consultants, etc.
are required which cost much time and energy and cause much
inconvenience. Thus, the alternative therapy of acupressure will be
suitable for treating insomnia in the elderly. Acupressure belongs to
the Traditional Chinese Medicine (TCM) as component of alternative
treatments [15].
It was defined as a technique which applies pressure on acupoints on
human body by using finger, palms or other devices to balance the vital
energy flows called Qi through meridians [7,16,17].
This traditional treatment is gaining increasing popularity due to its
non-invasive, non-side effect and home treatment nature. This paper
specifically focus on the elderly with insomnia while consider the
acupressure therapy. A systematical review was conducted to evaluate the
effectiveness of acupressure and summarize the treatment characteristic
as a preliminary study of acupressure therapeutic apparel development
for the elderly with insomnia.
To start with systematic
review, a literature search was conducted in March 2016 initially
focusing on any available published research papers about acupressure
for insomnia among elderly. Five databases including Medline, Science
Direct, CINAHL, Cochrane Library, Chinese Academic Journals were
accessed for paper searching using the Keywords: acupressure, acupoints,
traditional Chinese massage, insomnia, sleep quality, sleep disorders,
sleep disturbance, elderly, old people, silver group, aging people,
senior citizen. Besides, additional publications were identified through
other sources or hand searching.
A large number of research articles were collected
for first and second scans. Articles which are not quite related to
acupressure for elderly with insomnia must be excluded to simplify
further analysis. Exclusion criteria are set up referring these points
below:
- Duplications
- Randomized and controlled design: articles do not have a randomized controlled trial will be excluded
- Sample size: less than 30 will be excluded
- Acupoints: articles have not noted specific acupressure points on human body will be excluded
- Unsuitable symptoms: except insomnia, samples in research studies
have other serious diseases such as cancer, stroke, Alzheimer, etc.
should be excluded
- Unsuitable sample: studies focused on pregnant women, adolescents,
bed-ridden elderly, psychiatric patients, etc. but not active elderly
were excluded
- Unsuitable treatment: researches used needling acupuncture or used
acupressure as an assistant of other therapies should be excluded
- Others: articles which are too general or conduct research unconventional or unorthodox, etc. will be excluded
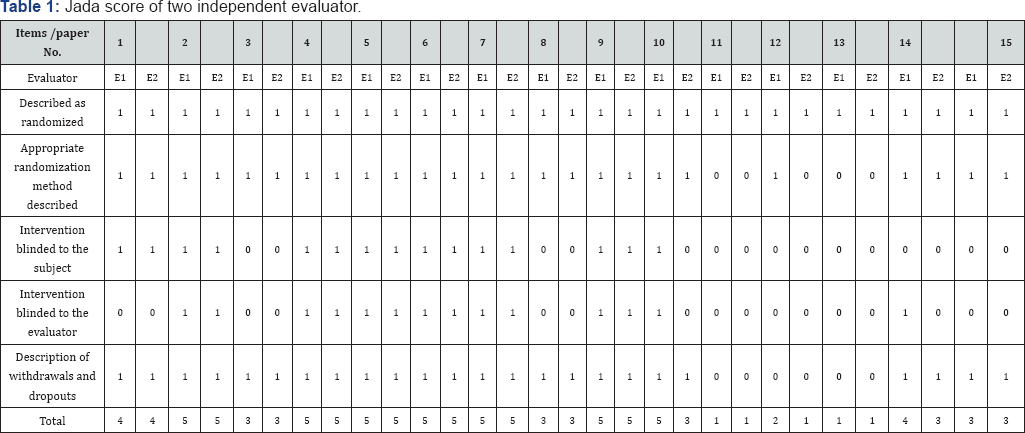
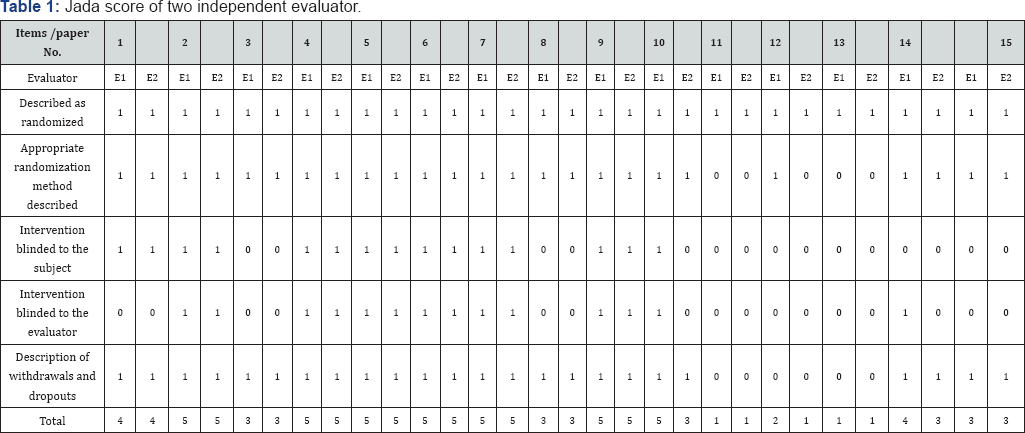
Two evaluators (Gong and Ameersing) independently assessed the quality of selected trials according to the modified Jada Scale [18]. There are five questions set up in the scoring system:
- Described as randomized?
- Appropriate randomization method described?
- Intervention blinded to the subject?
- Intervention blinded to the evaluator?
- Description of withdrawals and dropouts?
Answer to each question should be a “Yes” or a “No”
matching the score of 1 point or 0 point. Score of the modified Jada
scale could range from 0 to 5 that higher score indicates lower risk of
bias and higher quality of the trial.
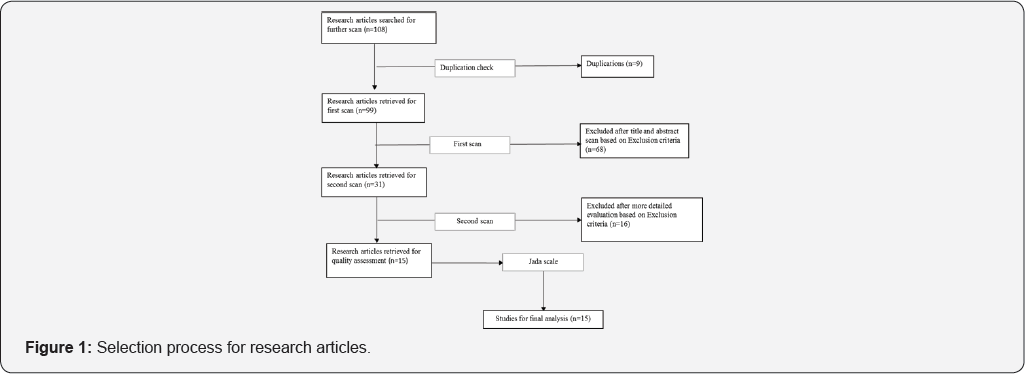
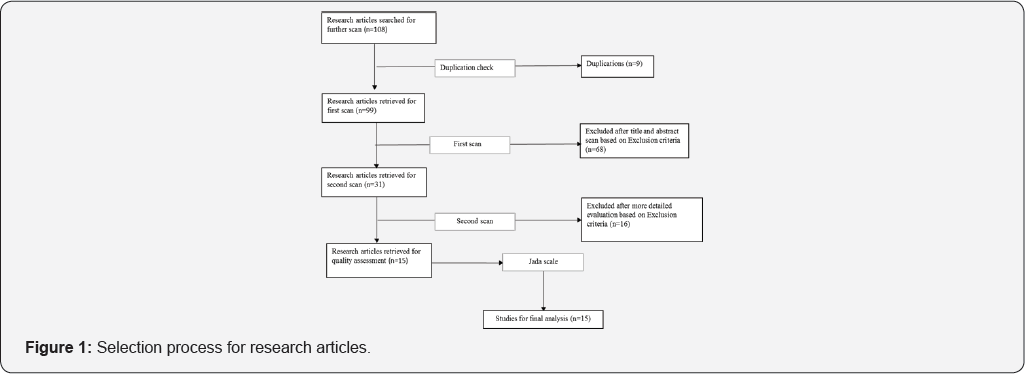
The literature search initially find 108 potential research articles for further scan based on the selection process in Figure 1.
Specifically, 9 articles were excluded after the duplication check.
Then the first san was conducted among the remaining 99 studies by
reviewing the titles and abstracts followed by the detailed evaluation
of the second scan. Totally, there are 93 articles excluded in the whole
scan process according to various exclusion criteria. Finally,
15clinical trial papers (3 from PubMed, 2 from Cochrane Library, 3 from
Chinese Academic Journals, 4 from Science Direct, 2 from CINAHL and 1
from other sources) are remained for further analysis.
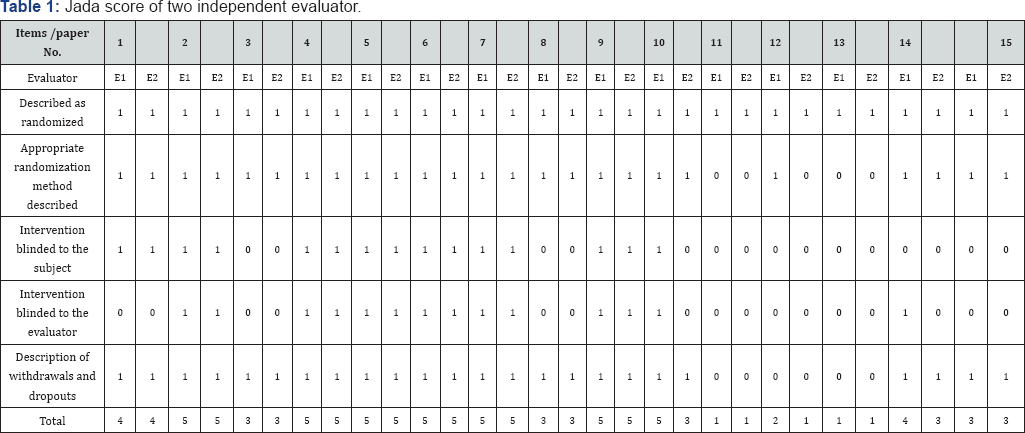
Note: E1, evaluator 1; E2, evaluator 2
All of these 15 studies were reported as randomized
clinical trials. The detailed scoring result of the modified Jada scale
given by two independent evaluators is presented in the Table 1
attached at the end. 80% of the reviewed studies had the Jada score
>3 that indicate a good quality with a relatively low risk of bias.
Moreover, 6 of these fifteen trails (study 2, 4, 5, 6, 7, 9) have got
the full mark of 5 from both evaluators. Only 3 trails (study 11, 12,
13) got the Jada score below 2 without blinded trail design and dropout
description. However, these 3 studies were all written in Chinese by
experts or doctors and conducted in hospitals or nursing home that still
have good referent value. The score variation may due to the theory
difference between Chinese and Western medicine.
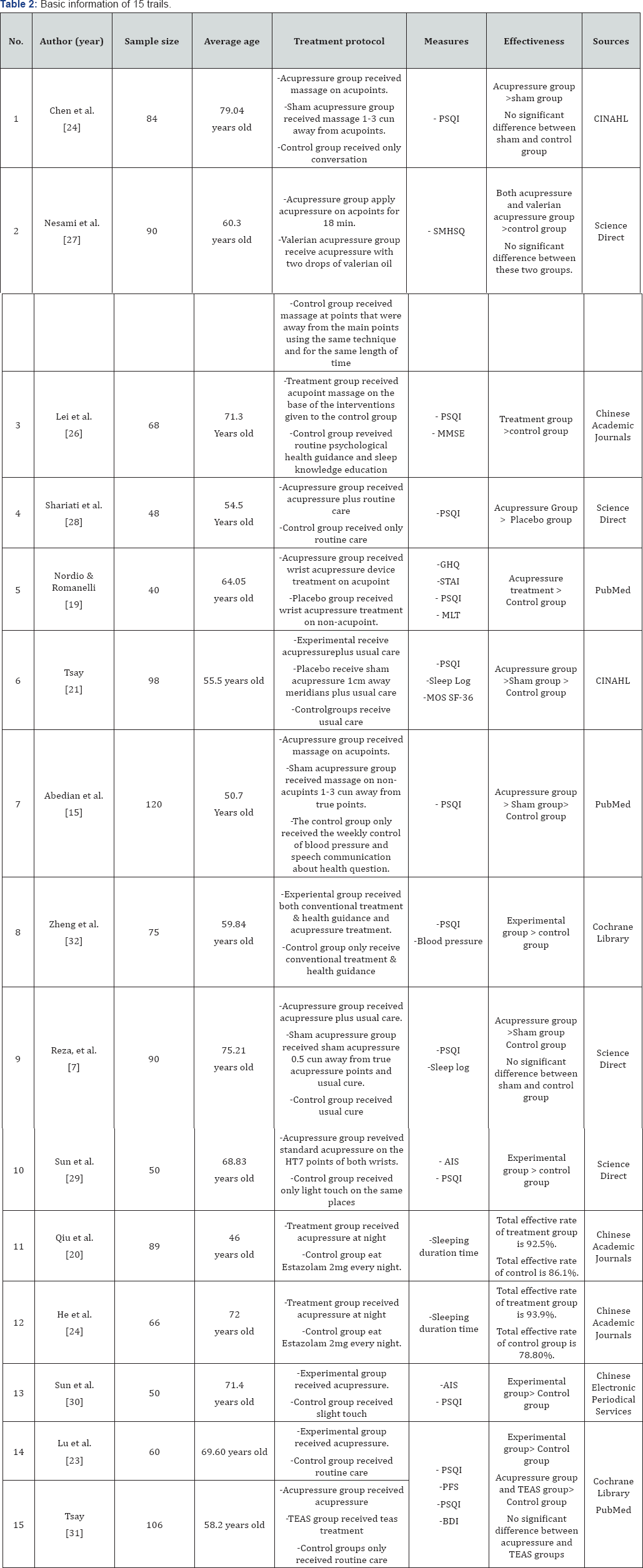
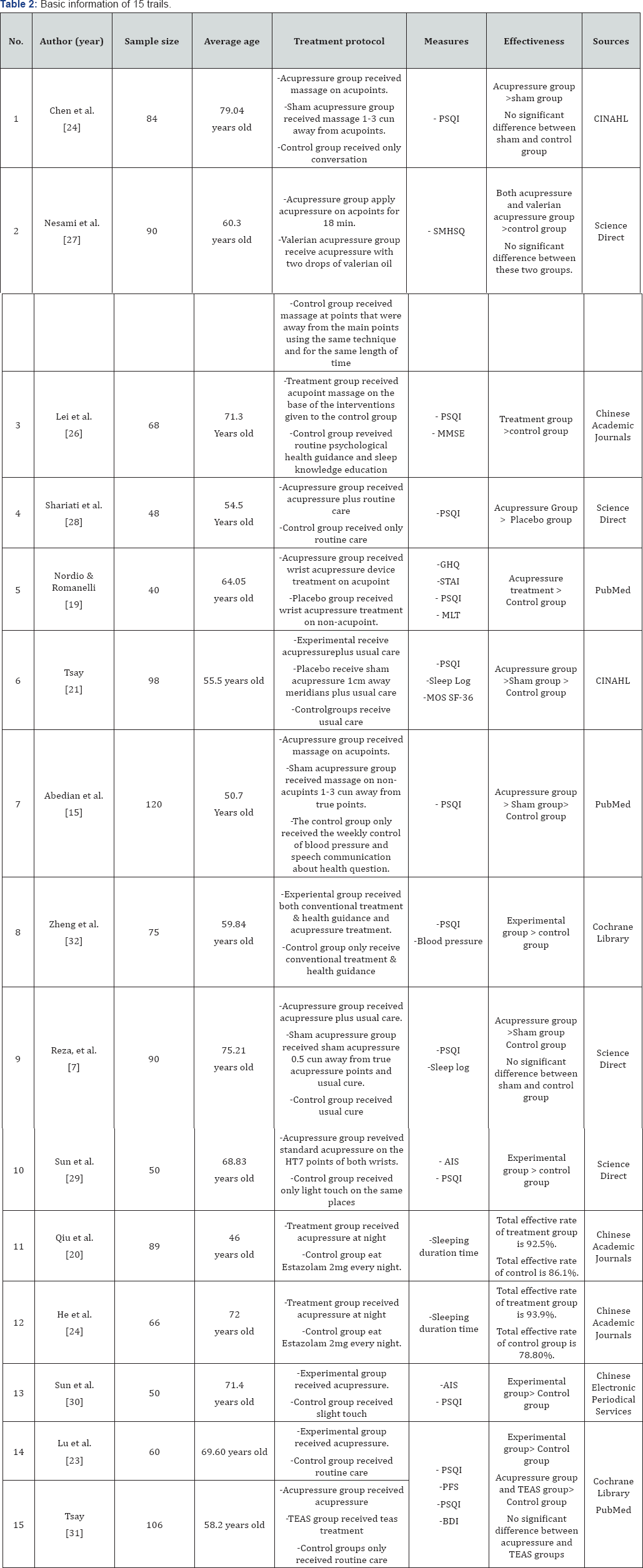
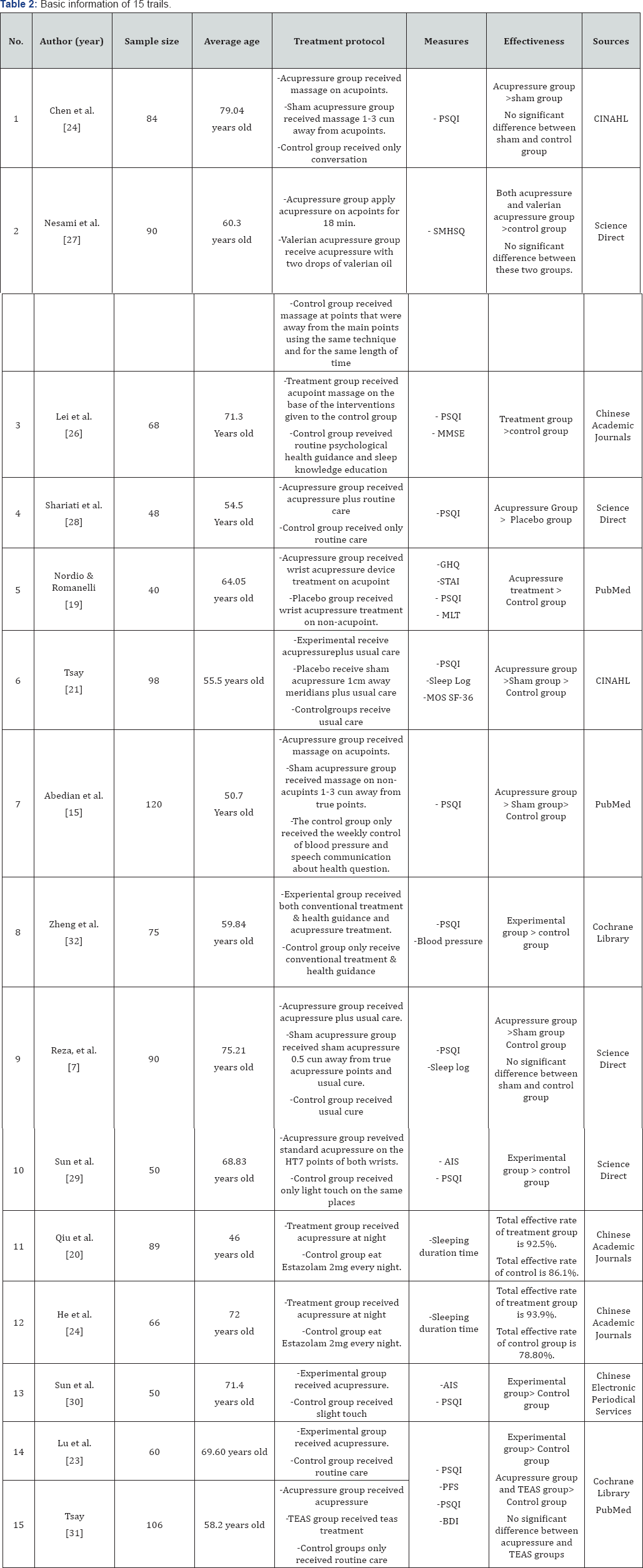
Note: RCT, Randomized Controlled Trail; CT,
Controlled Trail; PSQI, Pittsburgh Sleep Quality Index; SMHSQ, St.Mary's
Hospital Sleep Questionnaire; MMSE, mini-mental state examination; GHQ,
General Health Questionnaire; STAI, State-Trait Anxiety Inventory; MLT,
Urinary Melatonin; MRS, Menopause Rating Scale; AIS, Athens Insomnia
Scale; MOS SF36, Medical Outcome Study Short Form 36. TEAS,
Transcutaneous Electrical Acupoint Stimulation; PFS, Piper Fatigue
Scale; BDI, Beck Depression Inventory
Basic information ofthe 15 reviewed studies was summarized in Table 2.
Totally, there were 1134 insomnia patients included in trails with the
average age of 63.76 years old. All the trails indicated that
acupressure has a good therapeutic effectiveness on insomnia in the
elderly.
Two-arm clinical trail: A two-arm trail was
adopted by 9 of the studies (study 3, 4, 5, 8, 10, 11, 12, 13, 14) to
compare the outcome measures between or within two groups. Results
showed that compare to the control groups which received routine care
such as psychological health guidance, slight touch and sleep knowledge
education, treatment groups that received acupressure except usual care
were reported to be more effective (study 3, 4, 8, 10, 13, 14). To note
that study 5 conducted by [19]
set up a placebo group instead of a control group and use a wrist band
device instead of traditional finger pressure. Although a good treatment
effect has been received in the acupressure group, whether the placebo
group was effective or not remains unknown. Study 11 and 12 of [20] and [19]
compared the effectiveness between acupressure therapy and medication
therapy according to the Sleeping duration time before and after
treatment within each group. Results indicated that both acupressure and
medications have therapeutic effect on insomnia but acupressure was
found to be more effective. However, these two Chinese studies have not
adopt common western standardized outcome measures such as Pittsburgh
Sleep Quality Index (PSQI) and only present result by effective rate.
Although the effective rate definition was not standardized [18], this expression straightforwardly presented the improvement or reduction in treatment effectiveness.
Three arm clinical trial: Other 6 studies
adopted three- arm trail design by setting three groups for better
comparison. Except the acupressure group and control group, studies 1,
6, 7, 9 added a sham acupressure group by applying pressure on non
acupoints about 1-10cm away from true acupoints avoiding meridians. Two
of the trails (study 1 and 9) reported that acupressure was more
effective than both sham group and control group while there was no
significant difference between sham and control groups. However, results
of study 6 and 7 indicated that sham acupressure was more effective
than usual care in control group while acupressure treatment still have
the highest effectiveness. The therapeutic effect in sham group may
because the sham points were too close to the true points that still
within the effective area. Physiological or psychological effect also
works. Besides, the acupressure techniques used on non acupoints in sham
groups may achieve body relaxation which also leads to a better sleep
quality [15,21].
Another two studies (2 & 15) compared the effectiveness between the
mono therapy of acupressure and the combination therapy of Valerian
acupressure or Transcutaneous Electrical Acupoints Stimulation (TEAS).
It was reported that both the acupressure mono therapy and combination
therapy no matter acupressure with valerian oil or acupressure with
electrical stimulation had significant effectiveness in treating
insomnia in the elderly when compared to control groups.
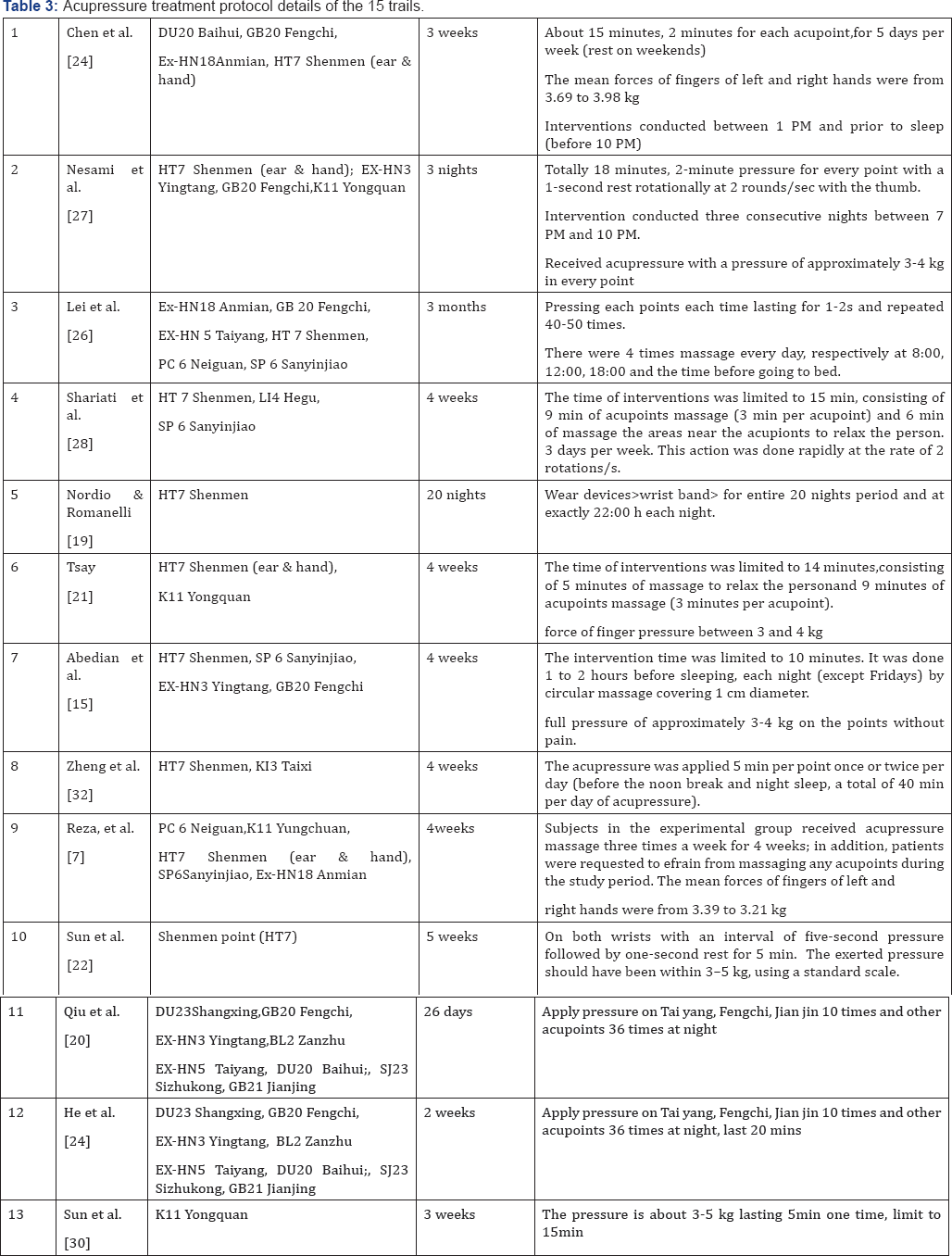
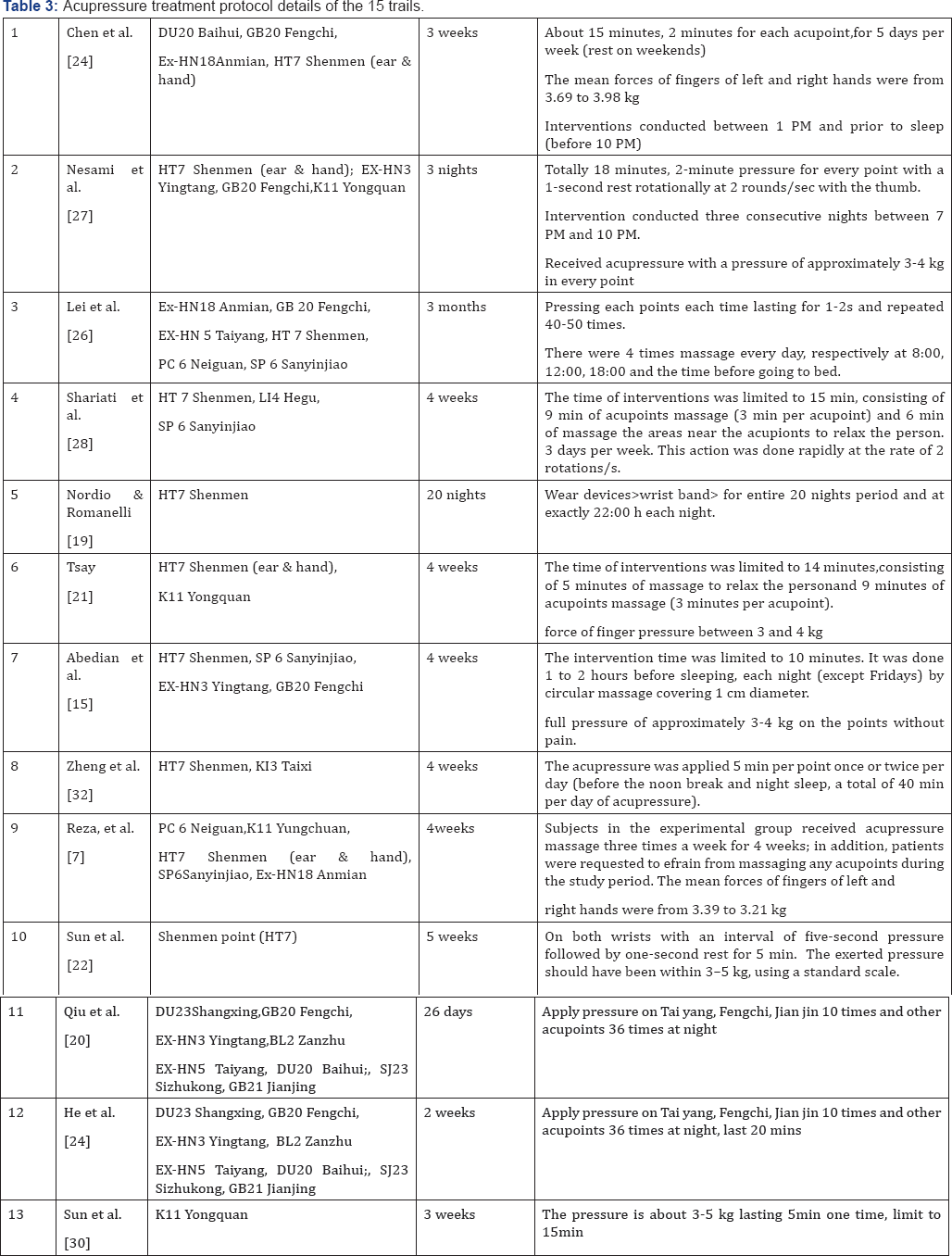
Acupressure treatment protocol details for insomnia of all the 15 studies were summarized in Table 3 regarding acupoints, pressure and specific interventions.
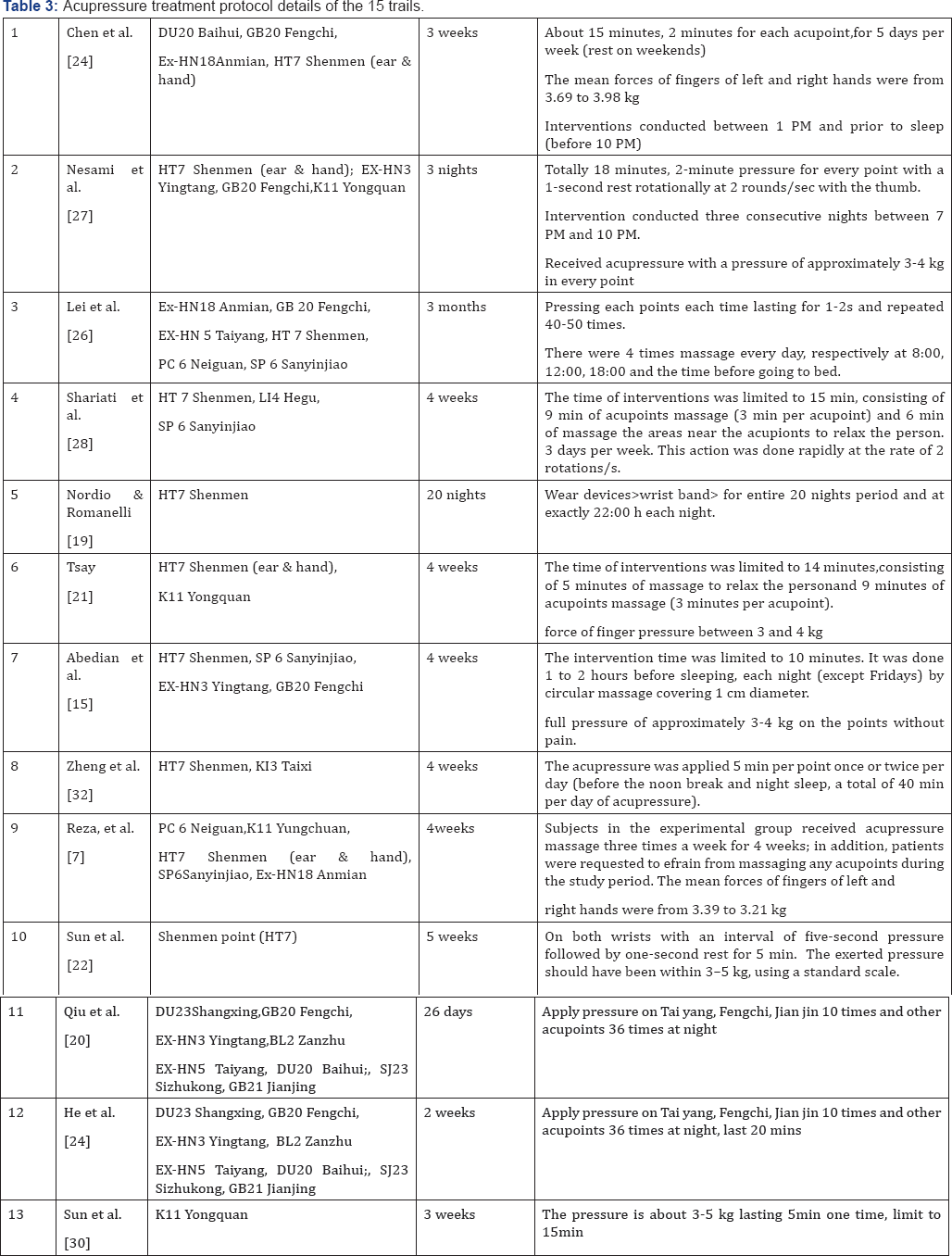
Acupoints: Totally, there were 18 core acupoints noted in these 15 acupressure trials with the frequency shown in Figure 2.
The most commonly used acupoint is the HT 7 (Shenmen) in hand with the
frequency of 11 followed by GB 20 (Baihui) on head and K11 (Yongquan) on
feet noted by 6 trials respectively. Besides, 50% of the 18 acupoints
concentrating on head including DU20 (Baihui), DU23 (Shangxing), GB20
(Fengchi), BL2 (Zanzhu), SJ 23(Sizhukong), EX-HN5(Taiyang),
EX-HN3(Yintang), Ex-HN18 (Anmian) and auricular HT 7 (Shenmen).

Pressure: A pressure need to be applied on
each acupoint with a specific force range when conducting the
acupressure intervention on human body. Too light pressure may have no
or little effectiveness on insomnia which was usually used in sham group
and have been proved to have no or little effectiveness on insomnia [22].
Otherwise, too much pressure may cause discomfort or even make patients
injured with bruising. According to the intervention information in Table 3,
the range of pressure force was usually between 3kg to 5kg. To explore
the most appropriate pressure force for various patients, the force
could be gradually increased from 3kg until the participant has a
tolerable sensation of soreness [23].
Intervention: Most of the trials stated detailed interventions as shown in Table 3.
To summarize, the mean duration of acupressure conduction lasted about
15min one time and 1 to 4 times per day. Each acupoint applied pressure
for 2 to 5 min with the frequency of 2-5 seconds pressure (2-3
rotations/s) and 1 second rest. Besides, many studies (study 1, 2, 5, 7,
8) suggested that it was better for patients to receive acupressure in
the afternoon before noon break or in the evening prior to night sleep.
Moreover, treatment period noted in the 15 trials ranged from 3 nights
to 3 months. Most of the studies conducted interventions for 4
consecutive weeks [24-32].
This systematic review evaluated the effectiveness of
acupressure for insomnia in the elderly and summarized the treatment
characteristics of this tradition Chinese medicine technique. Although
all of the selected acupressure studies see a significant effectiveness
on insomnia in the elderly, there still remain some limitations that
need to pay attention to. First, researches on acupressure for insomnia
are limited, a systematic review process could only find a few studies
that have reference value. Second, some of the studies especially those
written in Chinese have a relatively lower Jada score without blind
trial design and withdraw description. Third, when recruit participants,
the history of other interventions such as drugs have not been recorded
that might have some impacts on the results. Besides, some studies have
insufficient subjects for each separate subgroup analysis. Moreover,
more than half of the studies have not conduct a three-arm trial
including an acupressure group, a sham acupressure group and a control
group to minimize bias. Last but not the least, it is difficult for the
elderly or careers to find accurate true acupoints and conduct
appropriate intervention. In some trials sham acupoints were set too
close to true points that fail to have an effective comparison with true
acupressure group.
Consider the effectiveness, characteristics and
limitations of current researches on acupressure, recommendation could
be given as future directions of acupressure therapy and relevant
therapeutic garments development. We recommend that the 5 most effective
acupoints including HT 7 (Shenmen) on both hands, GB 20 (Baihui) on
head and K11 (Yongquan) on both feet could be regarded as design
reference considering their body locations. According to the result that
50% of the core acupoints concentrating on head, relevant therapeutic
garment such as head band, gorro could be designed. Before garment
design, investigation on a variety of requirements referring to human
comfort or device usability should be conducted via questionnaire or
interview to satisfy requirements of users. To note that physical
sensation of comfort on different part of the therapeutic garments
should be tested and adjusted when people wear it during different
locomotion or in different posture. Combination therapy of acupressure
such as herb acupressure, electrical acupressure, and heat acupressure
could be adopted in garments by smart textiles, metal yarns, mini
battery, etc. matching the meridians or acupoints on human body.
Moreover, acupressure force applied on each selected acupoint should be
tested while patients are static or dynamic. When the therapeutic
garment is developed, it is necessary to conduct a randomized control
trial with three-arm design (acupressure group, sham acupressure group
and control group) among suitable subjects to ensure the effectiveness.
Sham acupoints could not be too close to the true point in order to
avoid the effective area and main meridians. On the whole, acupressure
therapeutic garment has the potential to provide promising methods for
insomnia and highly improve the life quality of the elderly




Comments
Post a Comment