Corneal Defects and Stem Cell Therapeutics-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF INTELLECTUAL & DEVELOPMENTAL DISABILITIES
Abstract
This article explains important corneal defects/disorders; and therapeutic applications of stem cells for restoration of vital functions. This article also describes use stem cells and their transplantation for retrieving of corneal functions. This article also tries to explain cell culture methods for corneal organoid culture that include multiple corneal cell types and extracellular matrices. It also describes removal of corneal blindness by grafting with cadaveric tissues, maintenance of corneal transparency and restoration of corneal endothelial dysfunction and visual impairment. Present review presents new advancements made in the field of biocompatible substrates, bio-matrix, transplantation methods and micro-niche maintaining factors for restoration, repairing and healing of corneal epithelial cell successfully. This article suggests dire need to explore and design new biomaterials to make matrix based nano-structure constructs for corneal repair and regeneration.
Keywords: Congenital corneal defects; Corneal clouding; Cornea organoid cultures; Stem cell therapeutics
Introduction
Cornea is the most anterior segment of the eye that provides exquisite vision. This is transparent outermost surface of the eye, consisting of a stratified epithelium, a collagenous stroma and an innermost single-cell layered endothelium. Cornea is an important visual structure assists in providing a clear vision by refracting light onto the lens, which in turn focusing on the retina. It is a vital tissue that remains poorly protected from the environment and face toxic dust and heat exposure. Cornea acts as a major protective shield to the eye and represents two thirds of its refractive power. It is made up of a tough transparent tissue admitting and focusing light in the eye. The cornea has a secondary protective function, it control light, and is able to screen out ultraviolet light. It also serves to physically protect the eye by shielding it from germs and small particles. Cornea is located over the pupil, iris, and the anterior chamber. All of these are very delicate components which are vitally important to sight. Cornea contains self-renewal cells which possess enormous regeneration capacity. The cornea is able to recover quickly from minor scratches, but deeper scars can cause the cornea to lose transparency and impede vision (Table 1).
The cornea is an ectodermal/neural crest derivative formed through a cascade of molecular mechanisms to give rise to the specific optical features necessary for its refractory function. Moreover, during cornea formation and maturation, epithelial stem cells are sequestered to ensure a constant source for renewal in the adult [1]. Cornea is made up of three distinct cell layers of different developmental origins: the outer, epithelial layer develops from the ectoderm overlying the lens vesicle; whereas iter, the stroma and the endothelium have mesenchymal origin. Its stromal cell layer is self-renewing epithelium that contains resident stem cell population. Damaged corneal cells are continuously replaced by population of stem cells (SC) and aged epithelium layer is replaced throughout life. Cornea also faces limbal defects related to opacity and neovascularization. These are treated by epithelial stem cells reside in limbal stroma and the corneal –endothelium [2]. Moreover, during cornea formation and maturation, large population of epithelial stem cells is sequestered towards the local sites for providing a long lasting source for renewal in the adult [1].
The cornea is derived from ectodermal/neural crest cells and formed through a cascade of molecular mechanisms which provides it specific optical features which are necessary for refractory function. In addition, for repairing of cellular damage in cornea small number of stem cells found at the edge of the cornea, known as limbal stem cells are used for therapeutic purposes. These cells easily replace damaged ones, and repair injured part, once these cells may lost due to injury or disease, the cornea can no longer be repaired. This permanent injury may affect the ability of light to enter the eye, and results in a significant loss of vision. Thus corneal defects are directly associated with limbal stem cell (LSC) deficiency, a bilateral disorder [3]. Failures of corneal epithelial stem cell transplantation can result in painful and blinding disease of the ocular surface [4] (Table 1).
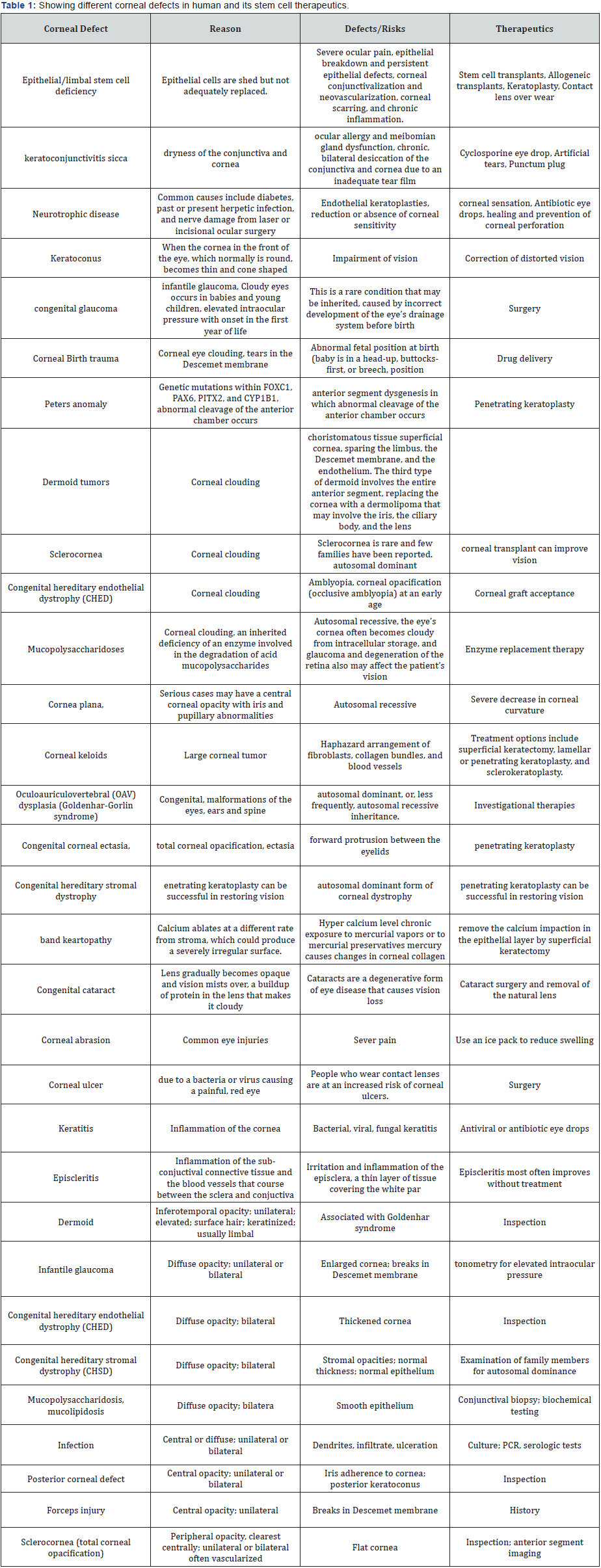
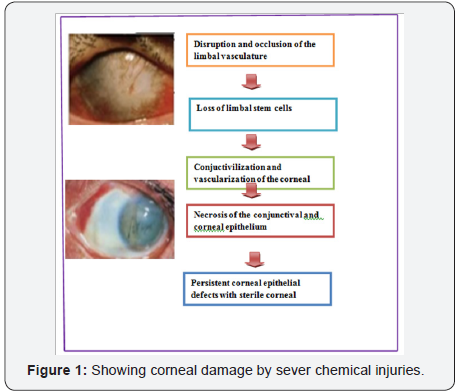
Mainly corneal epithelium or corneal epithelial layer get injured due to severe environmental stress mainly heat, light and high thermal temperature. All these factors results in dysfunction of transplanted cells and leads to reduction of visual clarity and loss of vision. These corneal epithelial injuries can be repaired by using limbal stem cells but it is very slow in diabetic patients. In case of extensive chemical burns or physically injured corneas only cure is limbal stem cell deficiency [5]. However, for corneal epithelial renewal and wound healing appropriate integration and coordination of cell signaling events are highly needful. In such cases, treatment may involve transfer of growth factor and normal adult stem cells to the ocular surface [6] (Figure 1). Topical tacrolimus treatment also cause significant decrease in corneal vascularization and reduce cellular inflammation in cells [7]. Similarly, insulin-like growth factor 1 (IGF-1) are also used to form three-dimensional ocular-like structures from hESCs [8].
Cornea contains keratocytes; these are quiescent mesenchymal stem cells of neural crest origin. The corneal stroma is large repository for stem cells. A small population of these cells resides in mammalian stroma that displays clonal growth, multipotent differentiation, and expression of an array of stem cell-specific markers. These corneal stromal stem cells (CSSCs) undergo extensive expansion without loss of the ability to adopt a keratocyte phenotype [9]. Stem cells also reside in the peripheral cornea and limbus. These peripheral and limbal corneal stromal cells (PLCSCs) are known to produce mesenchymal stem cells in vitro. Both corneal stromal and epithelial progenitor show Trans differentiation ability [10] and can be used for the treatment of many systemic lysosomal storage disorders [11]. For derivation and formation of various cell types from progenitor or stem cell of the keratocyte maintenance of niches is highly required. It also play important role in corneal regeneration [12]. Topical administration of eye drops is the major route for drug delivery to the cornea. It is extensively used in alkali-induced corneal wound [13]. Though, several therapies are currently in use for the treatment of persistent epithelial defects. Fibronectin is a naturally occurring glycoprotein found in serum that promotes cellular adhesion in wound healing [14]. Thymosin beta 4 (Tβ4) is a naturally occurring polypeptide secreted by inflammatory cascade cells. It plays an active role in promoting corneal wound healing. Non-preserved ophthalmic Tβ4 also known as RGN- 259 is used for treatment of nonhealing neurotrophic epithelial defects [15]. Topical ophthalmic Nexagon gel is applied for treatment of alkali corneal burns [16] (Table 1).
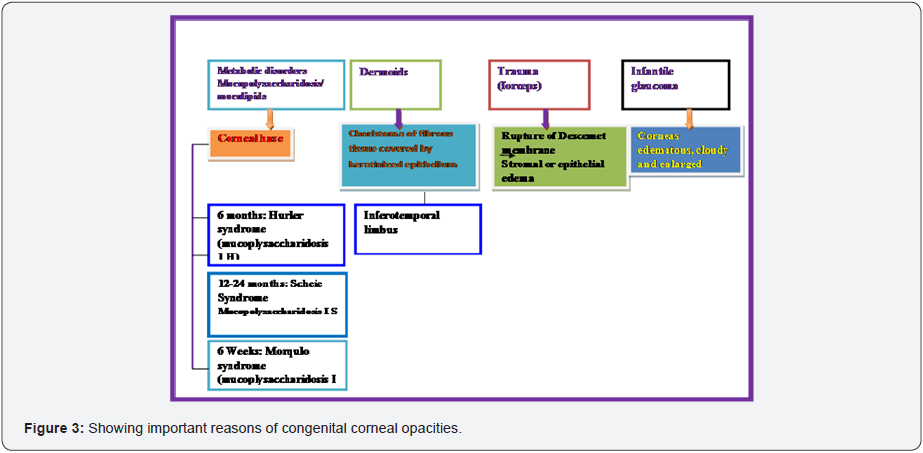
Corneal epithelial defects
Corneal epithelial defects are one of the most commonly seen ocular pathologies in the general patient population. Corneal epithelial defects are a focal loss of the corneal epithelium and can occur by a variety of reasons mainly due to mechanical trauma, corneal dryness, neurotrophic cornea and post surgical changes. Corneal epithelial defects accounted for 10% of all eye-related diseases sometimes with of systemic diseases or trauma both eyes are seen in patients. Several techniques exist for the management of corneal epithelial defects. For prevention of infection topical antibiotics are provided. For large defects, bandage contact lenses and pressure patching can be administered in patients. But long range healing is only possible through in vivo transfer of limbal stem cells which regenerate the corneal epithelium. Various genetic, metabolic, developmental, and idiopathic causes can result in congenital clouding of the cornea. A common reason for congenital clouding of the cornea is congenital glaucoma. Other major causes of corneal clouding include Peter’s anomaly, Dermoid tumors, sclerocornea, congenital hereditary endothelial dystrophy (CHED), mucopolys accharidoses and infectious/inflammatory processes. Other examples of congenital clouding of the cornea are sclerocornea, tears in the, descemet membrane secondary to birth trauma or congenital glaucoma, ulcers, metabolic, Peters anomaly, Edema (CHED). Epithelial/limbal stem cell deficiency constitutes a category of conditions in which epithelial cells are shed but not adequately replaced. Inflammatory disease, including kerato conjunctivitis sicca, may accompany any of the other condition. Most people fully recover from minor corneal abrasions without permanent eye damage. But deeper scratches cause corneal infections, corneal erosion, or scarring of the cornea. If these scratches are not treated properly, these create long-term vision problems. Healthy corneal epithelium is essential in protecting the eye against infection and structural damage to deeper tissues. Moreover, non-healing corneal epithelial defects can have other deleterious consequences, including infection, scarring, melting, and perforation [17] (Table 1). Common diseases of the cornea are keratitis, ocular herpes, herpes zoster and keratoconus. These conditions can damage the cornea, resulting in scars that interfere with vision by distorting light as it enters the eye. In Keratitis patients face sever inflammation, infection and ulceration of the cornea. Among important symptoms includes redness, blurred vision, discharge, severe pain, tearing and extreme sensitivity to light. Herpes zoster is skin disease caused by chickenpox virus but it spread to eyes can cause lesions on the cornea. There is seen ocular herpes infection caused by the herpes simplex virus. It causes sores on the cornea and is not curable. Keratoconus causes scarring, swelling and changes the shape of the cornea, creating distortions such as nearsightedness.
Diseases and disorders of cornea
Common diseases of cornea are keratitis, ocular herpes, herpes zoster and keratoconus. These conditions can damage the cornea. It form scars and interfere with vision by distorting light as it enters the eye. Keratitis causes inflammation, infection and ulceration of the cornea, and its symptoms include redness, blurred vision, discharge, severe pain, tearing and extreme sensitivity to light. Herpes zoster is an infection caused by the chickenpox virus. Ocular herpes viral infection (Herpes simplex virus), causes sores on the cornea and is not curable. Keratoconus causes scarring, swelling and changes the shape of the cornea, creating distortions such as nearsightedness, notes. Lysosomal storage diseases are important ocular problems which are caused due to degeneration, retinopathy, optic nerve swelling and atrophy, ocular hypertension, and glaucoma [18] (Table 1). Lysosomal storage disorder is a heterogeneous group of rare disorders characterized by abnormal accumulation of incompletely degraded substances in various tissues and organs. Corneal problems mainly cataract also caused due to accumulation of vitreous endosomal phosphoinositides [19].
Genetic defects
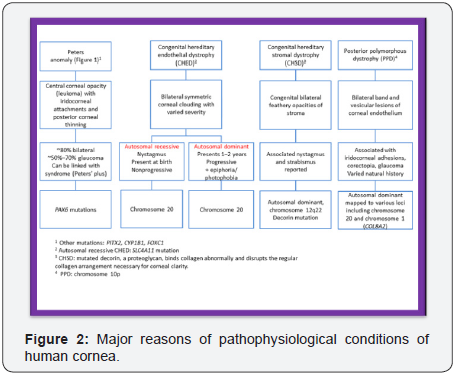
Corneal diseases also occur due to genetic defects. These defects also appear in phenotype mainly in form of cell types and the extracellular matrix released [20]. Defects in eye are also occurred due to somatic mosaicism of Pax6 mutation [21]. PAX6 is the key transcription factor involved in eye development in humans, but the differential functions of the two PAX6 isoforms, isoform-a and isoform-b, are largely unknown. To reveal their function in the corneal epithelium, PAX6 isoforms, along with reprogramming factors, were transduced into human non-ocular epithelial cells. Contribute to furthering the understanding of the molecular basis of the corneal epithelium specific phenotype [22]. Aberrant Pax6 gene affects corneal pathophysiology and corneal epithelial homeostasis [23]. Corneal abnormalities in Pax6+/- small eye mice mimic human aniridia-related Keratopathy [24]. Pax 6⁺/⁻ and PAX77(Tg/-) genotypes cause more severe corneal endothelial and stromal defects. Epithelial homeostasis of adult GFP-Dstn (corn1) corneas is abnormal, mimicking that of a normal conjunctiva or a pathological, conjunctivalized cornea. Corneal clouding, cataract, and colobomas are caused by missense mutation in B4GALT7 gene [25]. Micropinna microphthalmia mutation causes abnormal corneal epithelial cells [26]. In such animals abnormal protein accumulates in the endoplasmic reticulum (ER) of cells that normally express Fbn2 and causes ER stress [20]. It has been shown recently that the Mp mutation involves a chromosome 18 inversion that disrupts the Fbn2 and Isoc1 genes and produces an abnormal, truncated fibrillin-2(MP) protein. This abnormal protein accumulates in the endoplasmic reticulum (ER) of cells that normally express Fbn2 and causes ER stress. It was also shown that Fbn2 is expressed in the corneal stroma but not the corneal epithelium, suggesting that the presence of truncated fibrillin-2(MP) protein in the corneal stroma disrupts corneal epithelial homeostasis in Mp/+mice [26]. CYP1B1 gene alterations are also seen in primary congenital glaucoma individuals [27]. Cystinosis is caused by a deficiency caused by CTNS gene which sysnthesize lysosomal cystine transporter the cystinosin. It results in cystine crystal accumulation in tissues mainly in cornea (Figure 2).
EEC (ectrodactily-ectodermal dysplasia and cleft lip/ palate) syndrome is a rare genetic disease, autosomal dominant inherited. This disorder is caused by heterozygous mutations in TP63 gene. EEC patients showed ocular abnormalities [28]. It is treatable by using small interfering RNA (siRNA) by selectively silencing the mutant allele. Hh pathway is required during murine lens and cornea development [29]. An Hh signal promotes murine lens epithelial cell proliferation and disrupts fibre differentiation. Abnormal epithelial homeostasis occurs in the cornea of mice with a destrin deletion [30]. Dstn (corn1) mice lack normal destrin expression and develop corneal abnormality shortly after birth such as epithelial hyperplasia and total vascularization. Development of the eye depends partly on the periocular mesenchyme derived from the neural crest (NC), but the fate of NC cells in mammalian eye development and the signals coordinating the formation of ocular structures. Such defects in corneal development also occur due to defective migration of peri-ocular Nrp2+ neural crest/mesenchymal cells. Developmental and cellular factors also cause corneal epithelial dysgenesis in the Pax6+/- mouse model of aniridia [31]. Pax6 is the universal gene that regulates eye morphogenesis. Network of this gene (including Pax6/eyeless) create differences in morphology and structure of photoreceptor-type usage and lens [32]. It is also expressed in the ocular surface epithelium from early gestation until the postnatal stage [33]. Similarly, Lim2 gene also plays a critical role in establishing the correct internal refractive properties of the crystalline lens [34] (Table 1). Eye disorders are also seen after inactivation of TGF beta signaling in neural-crest stem cells [35]. LacZ (+) also affect cell movement during the development and maintenance of the murine corneal epithelium [36]. Mutations in the gene encoding the PtdIns3P 5-kinase PIP5K3/PIKfyve have been found in patients affected with François-Neetens fleck corneal dystrophy [37].
Inherited metabolic disorders
Several inborn errors of metabolism are seen in new borne babies [38]. Fabry disease is a rare X-linked inborn error of glycosphingolipid metabolism [39]. This is a multisystem X-linked disorder clinically characterized by angiokeratoma, corneal and lenticular abnormalities, acroparesthesia, and renal and cardiac dysfunction and stroke [40]. Conjunctival and retinal vessel tortuosity and corneal verticillata are frequently observed in Fabry disease. It also shows prognostic ocular changes which increase disease severity [41]. But lenticular changes are not seen, these are less common than that of corneal, conjunctival and retinal changes. Other corneal abnormalities range from the routine sequestrum and PPM-related opacity to those rare infiltrates accompanying inborn errors of metabolism (Glaze MB 2005). Mitochondrial fatty acid beta-oxidation in the human eye and brain also causes implications for the retinopathy of long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency [42]. Reduced energy generation in the choroid plexus may contribute to the cerebral edema observed in patients with beta-oxidation defects. Mucopolysaccharidosis type VI or Maroteaux Lamy syndrome is an autosomal recessive lysosomal storage disorder resulting from a deficiency of arylsulfatase B. This disease is characterized as hepatosplenomegaly, dysostosis multiplex, stiff joints, corneal clouding, cardiac abnormalities, and facial dysmorphism, with intelligence usually normal [43].
Corneal transplantation is best therapeutics for severe corneal disorders. It is the primary treatment option to restore vision for patients with corneal endothelial blindness. For transplantation purpose tissue-engineered corneal endothelial grafts are constructed by using cultivated human corneal endothelial cells. These can be isolated from cadaveric corneas and may serve as a potential graft source [44]. Corneal organoids that include multiple corneal cell types and extracellular matrices are also used for restoration of corneal defects [20]. However, cell replacement therapy and transplantation of stem cells are considered more effective corneal regeneration and reconstruction. Hence, there is an increasing demand of human corneal tissue for surface reconstruction and transplantation. Therefore, to fulfill corneal tissue grafts new innovative methods are being developed to supplement tissue donation. Due to insufficient cornea donation and inherent artificial lens problems, alternative treatment strategies based on stem cell transplantations for become boon for visually impaired newborns.
Corneal wound healing
Corneal wound healing is a complex process involving cell death, migration, proliferation and, differentiation. It also needs extracellular matrix remodeling. Many similarities are observed in the healing processes of corneal epithelial, stromal and endothelial cells, as well as cell-specific differences. Corneal epithelial healing largely depends on limbal stem cells and remodeling of the basement membrane. Many improved methods are developed for growing limbal stem cells in the laboratories which are highly feasible biomaterials for better transplantation. However, to overcome the limitations of stem cells new potential sources of stem cell derivation different approaches are applied. In the laboratory limbal stem cells can be derived from embryonic stem cells or induced pluripotent stem cells (iPS cells). These are used as endless source for generating large quantities of limbal stem cells for therapeutics of patients mainly those who want to avoid surgical operation and are in great need (Figure 2). Corneal organoids from human induced pluripotent stem cells are used to tackle with such abnormalities [20]. Corneal pathological effects related to one or all of the corneal layers that produce corneal opacity can be removed by using stem cells.
The mammalian cornea contains a population of basal epithelial stem cells which maintain homeostasis and continue repairing. Corneal stem cells are used to generate corneal cells for long term supply of source material [45,46]. These cells transform to precursor cells (epithelial cells) in spheroid cell culture [47] and develop in to keratocytes [48] and also participate in corneal regeneration [49]. Besides, conventional allograft therapy, corneal scarring method is also developed to avoid allograft rejection and to reduce complications related to endothelial failure. In explants culture, stromal cells are used as autofeeder layer and expansion of human corneal epithelial cells [50]. For deriving limbal epithelial stem cells for healing, a micro niche is needed for self-renewal of the corneal epithelial stem cells. In addition, few growth factors, stromal niche cells, and specific extracellular matrix compositions are also required to maintain this environment [51]. Moreover, cultured corneal epithelial cells are considered to be a promising material for constructing bio-artificial cornea [52]. Similarly, mesenchymal stem cells (MSCs) acquire certain characteristics of corneal epithelial cells [53]. These cells are isolated from non-corneal tissues for stem cell therapies of cornea. These cells show immuno-modulatory properties, and claims to trans-differentiation into corneal cells [54] (Figure 2).
Corneal endothelial dysfunction is a major problem in corneal transplantation. For healing endothelial cells need migration and spreading of cells after proliferation [55]. Tissueengineering based therapy of corneal endothelial dysfunction is available, in which HCECs are cultured on the PCM-DM because it provides a feasible xeno-free matrix substrate [56] for therapeutic purpose long term ex vivo culture is needed to generate enough cell numbers for transplantation [57]. Limbal biopsy-derived stromal cells (LBSCs) expanded rapidly in media containing human serum. These generate spheres expressing stem cell genes (ABCG2, Nestin, NGFR, Oct4, PAX6, and Sox2) [58]. LBSCs are capable of corneal stromal regeneration and can be used as potential source for autologous stem cells for treatment of corneal stromal blindness [58], while allogeneic limbal mesenchymal stem cell (LMSC) therapy is used for corneal healing after a severe chemical burn [59]. However, direct treatment of corneal scarring can be done by using autologous stem cells that can reduce the need for corneal grafts (Figure 2).
Restoration of corneal defects
The cornea is covered by a stratified epithelium that is renewed by stem cells located in the peripheral region of the cornea. It is known as the limbus. Stromal keratocytes found in the stroma of the limbus can be expanded in culture for obtaining limbal fibroblasts (LFs). These cells showed similar characteristics to bone marrow mesenchymal stem cells (BM MSCs). These are used to maintain the epithelial stem cell phenotype in the limbal region. The integrity and normal function of the corneal epithelium are essential for maintaining the cornea’s transparency and vision. There exists a population with progenitor characteristics in the limbus that maintains a constant epithelial repair and renewal. Currently, cell-based therapies are used in replacement of defective eye components mainly for restoration of visual receptors. These are also used for treating limbal stem cell deficiencies. For this purpose both cultured limbal epithelial transplantation and cultured oral mucosal epithelial transplantations are done. Besides this, sphere-forming cells are generated from peripheral corneal stem cells which are used as potential source of progenitor cells for treatment of corneal degenerative diseases [60].
Limbal fibroblasts showed a greater potential for differentiation into corneal epithelium. Similarly, tissue-specific adult progenitors show reprogramming capacity that is used for obtaining desirable cells types for therapeutic purposes [61]. But it will need more favorable environment at different stages of differentiation [61] otherwise there occurs a loss of cell lineage that may form lens placode and any other tissue [62]. However, new simple, reproducible, animal-material free methods are used for cultivating and characterizing cornea limbal epithelial stem cells (LESCs) on human lens capsule (LC) [63]. Both corneal epithelium and lens share a common pool of precursors [64]. Healthy corneal endothelium maintains corneal clarity. Once corneal endothelial get damaged and loss of cell count occurs it results in severe visual impairment. For this purpose barrier and pump functions are essentially normalized for the maintenance of corneal transparency and restoration of corneal endothelial dysfunction [65]. An elevated level of calcium and epidermal growth factors (EGF) aids in stem cell proliferation, regeneration and repair (Table 1).
Ciliary body is a good source of lens stem cells which are used for generation of corneal epithelium [66]. Human anterior lens capsule are used as a biologic substrate for the ex vivo expansion of limbal stem cells in ocular surface reconstruction [67]. There are many ocular surface disorders that are caused due to damage in the limbal region that results in destruction and a deficiency of corneal stem cells. For lens regeneration, induction of trans-differentiation in pigment epithelial cells is highly needful in stem cells bioengineering [68]. Moreover, for treatment for ocular surface diseases limbal transplantation or cultivated limbal cell transplantation are usually done [69]. Other methods that are followed for control of ocular disease and prenatal genetic eye related genetic disorders preclude ocular stem cell populations based lentiviral vector-based gene transfer [70]. More specifically, multipotent cells found within the iris pigment epithelium (IPE) [71] are used for regeneration of lens tissue in newts because of their developmental plasticity. Similarly, neural retinal regeneration occurs in the anuran amphibian Xenopus laevis during post-metamorphosis follows trans differentiation of retinal pigmented epithelium [72]. Moreoften, for cell replacement therapy reprogramming of cells from one tissue type to another needs manipulation of expression of transcription factors. These reprogrammed cells [73] induced by certain transcription factors maintain apoptosis and may involve in the perforation of the cornea in patients [74]. These cells can be used for therapies for many human diseases.
Maintaining stem cell microenvironment
Micro-environment supports differentiation of stem cell progenitors which form epithelial cellular sheet for repairing and wound healing. It is an important factor which is required for maintenance and regulation of stem cells. More specifically, limbal stromal cells are also used to maintain niche in vitro cocultures [75]. Human limbal epithelial cells (HLE) and corneal stromal stem cells (CSSC) reside in close proximity in vivo in the corneal limbal stem cell niche. Thus, limbal stromal cells with an intact cell-cell contact help to maintain LSCs in an undifferentiated state in vitro during expansion. These need specific tissue environment (niches) similar to stem/progenitor cells reside in eye. RAFT TEs are also used for restoration of limbal niche following ocular surface injury or disease [76]. For therapeutic purposes mesenchymal-like stem cells are derived from limbal area of the corneal stroma [77]. Limbal epithelial stem cells (LESCs) also need specific niche to maintain the transparent ocular surface required for vision. This micro-niche is also provided by limbal crypts niche for the resident LESCs and associating and dendritic pigmented limbal melanocytes and elongated limbal stromal cells [78].
Similarly, niche environment is also provided by amniotic membrane for cultured LSCs. LSCs have proved effective in the treatment of highly difficult human wounds, such as diabetic ulcers, recalcitrant chronic wounds, and even persistent epithelial defects of the cornea but these cells need limbal-like environment for the transplanted area of cornea [79]. Cord lining stem cells are also used in cell therapy and regenerative medicine [80]. Corneal epithelial stem cells are located in the limbus, the junction between the cornea and the conjunctiva. These can be used for formation of epithelial sheets for the treatment of limbal stem cell deficiency [81]. Stem cell niche is also maintained by physically protected microenvironment in close proximity to a variety of neighboring niche cells. Design and recreation of elements of various stem cell niches mainly 3-dimensional niche architectures can be used for having more biocompatible substrates, matrixes, sheets and factors which can be used for creation of defined topographical features in stem cell derived tissues and make them more applicable for numerous tissueengineering applications [82].
Maintenance of microenvironment in cell culture is highly important for regulation of interactions of various factors and stem cell function. It is also essential for maintaining cellular differentiation, corneal transparency, vision and ocular surface reconstruction [83]. It is also required for restoration of important signaling pathways for differentiation of epidermal/ epithelial cells to derive specific epithelial cell types [84]. Similarly, limbal niche is required for differentiation of limbal stroma [85] after an injury [86]. Further, for derivatization of tissue-specific stem cells and secretion of regenerative factors and matrix components stem cell microenvironment should be maintained for larger therapeutic successes [87]. In maintenance of microenvironment extracellular matrix plays a central role in regulating stem cell behavior, corneal differentiation, and participation in corneal wound healing. These are micro-mini factors which participate in various cellular processes and decide cell division patterns in corneal stem cell populations whether stem cells divide asymmetrically or symmetrically. There are certain factors which maintain environmental signals such as cytokines and growth factors and regulate corneal epithelial stem cells when used for corneal wound healing [88].
Stem cell therapy
Stem cells are self renewal cells which enormously divide to form to any cell type. These are used as a source of new, healthy specialized cells to replace damaged cells in the eye. There are several stem cell types which could be used in different ways, depending upon the particular disorder to be treated. Stem cells are used in conventional corneal transplantation, to restore cellular layer of the cornea [89]. These cells are used for replacing the lost retinal ganglion cells and restoration of photoreceptors. Besides this, engineered transplantable stem cells are also transferred for therapeutic purposes to restore patient-specific cornea or lens functions [90]. These cells possess enough potential for the production of new biological components mainly cornea and are best tools for regenerative medicine. These cells are used for treatment of various eyespecific pathologies mainly in retinal degenerative diseases. Normally mammalian cornea contains a population of basal epithelial stem cells which maintain cornea homeostasis and repair [91] (Table 1).
Induced pluripotent stem (iPS) cells are also used to replace defective optical tissues and cells. These cells can be derived from autonomous fibroblasts by using multiple ectopic transcription factors in culture medium. Recently, ciliary body epithelial cells (CECs) are identified as a new cell type for iPS cell generation that has higher reprogramming efficiency in comparison to fibroblasts [92]. Besides, interstitial celltelocyte which possesses outgrowth prolongations named as telopodes which form heterocellular networks are also used for therapeutic purposes [93]. Human umbilical mesenchymal stem cells are used to tackle with corneal defects [94]. These (UMSCs) are transplanted into the corneal stroma participate both in extracellular GAG turnover and enable host keratocytes to catabolize accumulated GAG products. These, cells are therapeutically highly useful for treatment of corneal defects associated with MPS and other congenital metabolic disorders. Human iPS cell-derived organoids through sequential rounds of differentiation programs. These organoids share features of the developing cornea, harboring three distinct cell types with expression of key epithelial, stromal and endothelial cell markers. Similarly, corneal organoid cultures are also used for corneal developmental in diseased conditions. Similarly, stem cells found in corneal limbal region need specific microniche [95].
Keratocytes are potentially used for restoration of vision and have enlarged biomedical engineering applications. But these specialized cells can not readily expand in vitro. Though culturing corneal keratocytes is very difficult because keratocytes growing in a monolayer rapidly lose their stellate morphology and cease to express keratocyte markers such as keratocan, lumican and aldehyde dehydrogenase 1 family, member A1 (ALDH1A1) [95]. Derivation of keratocytes from human embryonic stem (hES) cells is used in cell-based therapy mainly for remove off corneal blindness. Mainly human fetal keratocytes (HFKs) start differentiation into neural crest-derived tissues when challenged in an embryonic environment [96]. Keratocytes can be generated from hESC cells, maintained and expanded in feeder-free culture medium. These first differentiate into neural crest cells by using the stromal-derived inducing activity of the PA6 mouse embryonic fibroblast cell line [97] (Figure 2).
Human corneal endothelial cells (HCECs) shows limited proliferative ability in vitro. Human bone marrow-derived mesenchymal stem cells (MSCs) (MSC-CM) proliferate in conditioned medium consistently and expand. Basal layer of corneal epithelium can repair epithelial cell damage but these could not regenerate in vivo. Stem cell population found in corneal stroma is heterogeneous in nature and show similarity with neural crest progenitor cells. These cells are also used for surgical treatment of fungal keratitis [98]. Stromal stem cells show biocompatibility in grafts and make sheets of decellularized human corneal stroma with or without the re-cellularization [99]. Both stromal cells and epithelial cells may act in concert in the cornea [100]. Interactions between stromal and epithelial cells play important roles in the development, homeostasis, and pathological conditions of the cornea [100] (Table 1). Optic stem cell therapy seems a good best hope for regeneration of permanently damaged cells. However, its treatment needs continuous drug treatments or other exogenous biomaterial implants depending upon the relevant ophthalmological condition (Figure 3).
Human embryonic stem cells (hESCs)
Human Embryonic Stem Cells (hESC) are used as important resource to obtain any differentiated cell type of the human body [101]. These cells are also used for development of lens and its regeneration [102]. These cells differentiate to form human trabecular meshwork and are used in therapeutics of glaucoma [103]. Umbilical cord blood mesenchymal stem cells are also used for transplantation purpose to replace injured corneal endothelium. These cells behave like human corneal endothelial cells (HCEC) and show ability to heal ex vivo corneal wounds [104]. These cells are used to replace damaged or diseased corneal endothelium [104] but cell transplantation needs specific micro environmental conditions for repairing and wound healing. hEScs stem cells become an important resource which can provide a limitless supply of any differentiated cell type of the human body.
Pluripotent stem cells
Pluripotent stem cells are self renewable cells which form functional keratocytes that are used for treatment of corneal stromal opacities. For their differentiation in vitro co-culture of mouse PA6 fibroblasts is required in the same medium [105]. Similarly, induced pluripotent stem (iPS) cells are also used for generation of corneal epithelial cells [106]. Similarly, human adult corneal limbal epithelial cells (HLEC) could be derived from iPS cells (L1B41) in presence of Yamanaka 4 factors [106]. This strategy is used highly successful for generation of corneal epithelial cells from human iPS cells. This is purely epigenomic in origin in which certain exogenous factors may induce differentiation of epithelial cells into corneal epithelial cells [106].
Mesenchymal stem cells/multipotent marrow stromal cells (MSC)
Mesenchymal stem cells are multipotent, non-hemopoietic cells, self-renewable cells which found in various tissues. These cells are expanded in vitro conditions and trans-differentiate into other type of cells. These cells reside in bone marrow (BM), support homing of hematopoietic stem cells (HSCs). These cells are used for repairing of tissues/cells essentially those originating from mesoderm. These cells indirectly assist in modulating inflammatory and immune responses and used for treatment of various pathological conditions especially for corneal reconstruction [107]. Mesenchymal stem cells obtained from diverse tissues show immunosuppressive and pro-anti inflammatory characteristics [108]. Mesenchymal stromal cells (MSC) are quite similar to bone marrow-derived mesenchymal stromal cells (BM-MSC). These cells are grown from the limbus of the human cornea [109]. These cells can be used as supportive cells to facilitate hematopoietic stem cell engraftment and to minimize the deleterious consequences of graft versus host disease by their immunosuppressive function.
Mesenchymal stromal/stem cells (MSCs) are promising stem cell type. These stem cells exist in different parts of the eye and are used for corneal wound healing and therapeutics [110]. These cells show robust osteogenic differentiation capacity and are used in healing/repairing of cutaneous defects due to burns or ischemic strokes. Certain induction factors are required that could induce trans differentiation of stem cells into corneal epithelium-like cells in vitro co-culture with immortal corneal epithelium cells. These cells are used as a potential source for ocular surface regeneration [111]. However, for development of corneal endothelium proliferating cells should express progenitor markers [112]. Human limbal epithelial cells (hLECs) are obtained from organ culture of corneal-scleral (OCCS) rims for therapeutic purposes [113]. In addition, spheroids of rabbit and mouse corneal stromal cells (CSCs) are also generated in vitro for reprogramming, bio-printing and tissue engineering [114]. These positively express the mesenchymal and stem cell phenotypes.
Mesenchymal stem cells (MSC) are promising source of stem cells which are used for corneal healing and regeneration. Mesenchymal stem cells reside in the murine corneal stroma [115] differentiate into chondrocytes and neurocytes are used to treat keratopathies. Corneal limbus (L-MSCs) is potential source of these cells which are required for corneal repair. MSCs participate in tissue repairing by modulating excessive immune responses in various diseases. These cells show wider therapeutic applications in murine models [116]. MSCs are used in therapy for a number of ocular surface diseases where inflammation plays a key role [116]. Cultivated limbal epithelial transplantation is done to restore ocular surface burn [117]. Human limbal mesenchymal cells (LMCs) are used to support the expansion of human corneal epithelial stem/progenitor cells (LSCs) in culture [118]. More specifically, multipotent human limbal stromal cells resembling mesenchymal stromal cells (MSC) show very high therapeutic potential [119] and facilitate the regeneration of injured tissue [120]. Further, both MSCs and its derived factors are used to treat diseases of the cornea and other tissues [120]. These cells may be a good source for bioengineering of corneal tissue and for cell-based therapeutics.
Bone marrow mesenchymal stem cells are administered to repair injured cornea mainly for its reconstruction, but not to the normal cornea. Similarly, systemically injected syngeneic mesenchymal stem cells (MSCs) used in transplanted cornea, suppress induction of alloimmunity, and promote allograft survival [121]. But for proliferation and development of rapid corneal epithelial regeneration these cells required specific stem cell (SC) niche [122]. However, expression of stage-specific embryonic stem cell (ESC)-like properties of these cells can be used for new cell based therapeutics [123]. Mesenchymal stem cells (MSCs) differentiate into different cell types such as fibroblasts, adipocytes, cardiomyocytes, and stromal cells. These cells display properties similar to mesenchymal stem cells and demonstrate the ability to reproduce an organized matrix in vitro. These cells express surface molecules like CD13, CD29, CD44, CD73, CD90, CD166, CXCL12 and toll-like receptors (TLRs) [124]. CSSCs have shown great potential for the development of cell-based therapies for corneal blindness and stromal tissue bioengineering [125]. These cells pass through a correct specification of cell lineages that is essentially needed within the developing cornea for normal vision [126]. Besides, stem cell therapy, there is a need to develop alternative treatment regimens for congenital corneal diseases of genetic mutation [127]. Keratoplasty is most effective treatment for corneal blindness, but there is a shortage of donated cornea that prevents corneal transplantations.
Umbilical cord mesenchymal stem cells (UMSCs)
Umbilical cord mesenchymal stem cells (UMSCs) were found successful in repairing of corneal defects in mice [128]. These cells possess unique immunosuppressive properties and are proved highly valuable tools for cell therapy [94]. Umbilical mesenchymal stem cells can be easily isolated, expanded and stored in liquid nitrogen, and can be quickly recovered from when a patient is in urgent need. UMSCs exposed to inflammatory cells synthesize a rich extracellular glycocalyx composed of the chondroitin sulfate-proteoglycan versican bound to a heavy chain (HC)-modified hyaluronan (HA) matrix (HC-HA). This matrix also contains TNFα-stimulated gene 6 (TSG6), the enzyme that transfers HCs to HA, and pentraxin-3, which further stabilizes the matrix. Similarly, adipose-derived stem cells (ADSC) express keratocyte-specific phenotypic markers and express corneal-specific matrix components when these are cultivated under conditions which support and induce differentiation in corneal stromal stem cells to form keratocytes [129]. Human adipose-derived cells (hASCs) found overlaid on scleral contact lens (SCL) act as carrier and proliferate to finish ocular alkaline burn [130] (Figure 2). ADSC are potentially used in corneal cell therapy and tissue engineering [129]. Similarly, adipose-derived mesenchymal stem cells (ADMSCs) differentiate into corneal epithelium-like cells after transfection with Pax6 gene [40]. These become a good source of generating corneal epithelium-like cells for construction of tissue engineered cornea TECE transplantation aids in corneal transparency and thickness, while stem cell therapy can restore corneal endothelial dysfunction [131] (Figure 2). Similarly, human bone marrow mesenchymal stem cells (hMSC) are allowed to differentiate after inducing into epithelial-like cells to seek corneal epithelial-like cells. These cells are used in corneal tissue engineering [132]. By using human corneal stromal stem cells (dhCSSCs) dorsal root ganglion neurons (DRG) can be differentiated that can restore normal cornea functions [133].
Mesenchymal stem cells trans differentiate into corneal epithelial cells restore experimental limbal stem cell deficiency in rabbits [134]. More often, modulatory effect of rat bone marrow mesenchymal stem cells (MSC) on human corneal epithelial cells (HCE-T) is stimulated with pro-inflammatory cytokines interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α) [135]. Further, different factors, such as TGF-β, IL- 10, IDO, PGE-2, sHLA-G5, HO, and Galectin-3, secreted by Certain other factors such as Sox2, Oct-4 and Nanog are also required for AMSCs differentiation into neuronal-like cells. These AMSCs are promising source for stem cells and are extensively used in the field of regenerative medicine [136]. Meanwhile after mesenchymal stem cell transplantation expression of ABCG- 2, needs β(1)-integrin and connex in 43 for maintaining their stem cell character so as to these cells could transdifferentiate into epithelial progenitor cells. In addition, other putative factors secreted by MSC also assist in therapeutic use mainly in corneal repair [137]. Moreover, for in vitro colonization in vitro mesenchymal stem cells from Human adipose tissue (h-ADASC) needs PEA-based copolymers in combination with extracellular matrix coatings. Further, feasibility of adiposederived mesenchymal stem cells (ADMSCs) that differentiate into corneal epithelium-like cells after transfection with Pax6 gene is also being checked [40]. Macroporous membranes composed of the optimal PEA subtypes and coating proteins are tested after implanting them inside rabbit cornea [138].
The corneal epithelium is maintained by the limbal epithelial stem cells (LESCs). These cells found in basal layer of the limbus that occurs in a narrow transition zone segregates the peripheral cornea from the adjacent conjunctiva. These cells essentially require a specific microenvironment or limbal cell niche that can generate stromal cells similar to fibroblasts [139]. Similarly, bone marrow mesenchymal stem cells (MSCs) transdifferentiate into corneal epithelial cells and are used in limbal stem cell deficiency (LSCD) [140]. However, human corneal epithelium self-renewal is maintained by setting a regular niche microenvironment in the limbus [141]. It is also required for vascular regeneration of corneal and retinal cells [142]. MSCs induction by CSCs that transdifferentiate into corneal epithelial cells also needs presence of fibroblast growth factor 2 and transforming growth factor β for maintain microenvironment to form endothelialmesenchymal transition (EnMT). This endothelial wound-healing is also maintained by cell migration toward artificial wound defects mediated by p38 and c-Jun N-terminal kinase [143]. In addition, certain factors support the regenerative function of human limbal epithelial progenitor cells (LEPs) during wound healing are also required [144].
Mesenchymal stem cells (MSCs) reside in different body tissues and can be obtained from bone marrow, skeletal muscle, dental pulp, bone, umbilical cord and adipose tissue. MSCs are used in regenerative medicine mainly based on their capacity to differentiate into specific cell types. These cells can form many cell types such as retinal pigment epithelial cells, human corneal keratocytes, human osteosarcoma and microvascular endothelial cells by exposing them with different physical chemical factors [145]. However, post-operative injection of MSCs could inhibit keratoplasty rejection and prolong the corneal allografts survival in a rat model [146]. These are promising candidates for immune modulator therapy. These were found successful in several organ transplant rejection models [147]. These act as bioreactors of soluble factors which promote tissue regeneration in damaged tissues. These (MSC) cells perform distinct functions such as prompting wound healing, and show anti-inflammatory and immunoregulatory ability. MSCs show immunoregulatory capacity and elicit immunosuppressive effects in a number of situations. These are immune privileged cells, which display low expression of class II Major Histo compatibilty Complex (MHC-II) and its costimulatory molecules on cell surface. These cells also interfere in different immune pathways to respond by means of direct cell-to-cell interactions and soluble factor secretion [148]. MSC are also used for treatment of many ocular diseases, such as corneal diseases, uveitis and retinal diseases [146]. These are most appropriate candidates used in cell therapy and potentially used in veterinary regenerative medicine [149].
Mesenchymal stem cells (MSCs) are used to contruct ocular surface and are sub-conjunctivally administered on corneal wound healing in the acute stage of an alkali burn [150]. These are widely used in tissue engineering, immunology, gene therapy, and oncology [151]. MSCs significantly accelerate corneal wound healing and attenuate inflammation and reduce CNV in alkaline-burned corneas. These cells influence cell proliferation and growth factor expression of corneal limbal epithelial cells (LECs) in vitro [152]. Further, down-regulation of MIP-1α, TNF-α and VEGF influence cell proliferation [150]. Similarly, SDF-1α-induced progenitor cell recruitment and macrophage VEGF production plays critical role in the experimental corneal neovascularization [153]. In addition, systemic administration of adult stem/progenitor cells (MSCs) reduces inflammatory damage to the cornea without engraftment and primarily by secretion of TNF-α stimulated gene/protein 6 [154].
Mesenchymal stem cells generate potential beneficial factors that make corneal recovery possible. For this purpose MSCs are seeded on a xenogeneic acellular corneal matrix (ACM) in vitro [146] in a suitable microenvironment. The secreted corneal matrix can be used as a substitute for healing corneal wounds [146]. MSCs induce cell to cell interaction and generate immunomodulatory effects on innate and adaptive cells of the immune system [124]. Both cell-cell contact inhibition and transforming growth factor-beta2 (TGF-β2) in aqueous humor may be responsible for maintaining human endothelial cells in a non-replicative state in vivo [155]. Contrary to this, human limbal explants can be generated in a cholera toxin-free medium with no feeder cell layer [156]. Allogeneic cultivated limbal epithelial cells using human amniotic membrane as a carrier are also transplanted into the recipient eye for restoration of visual defects [157]. Limbal basal epithelial cells also serve as niche cells and generate progenitors with angiogenesis and mesenchymal stem cells potentials. These cells participate in angiogenesis and regeneration during corneal wound healing [158]. Superficial limbal explants are also used to promote the surgical treatment of fungal keratitis [159].
Neural colonies (neurospheres) can be generated from adult corneal limbus in vitro but these require setting of a suitable microenvironment [160]. Naturally such niche is found at corneoscleral junction of the eye that inhabits limbal epithelial stem cells and plays critical role in maintaining stem cell differentiation [161]. These cells facilitate corneal epithelial regeneration by providing physical support and chemical signaling [158]. Besides, MSCs human amniotic membranes ex-utero derived stem cells are also used for corneal therapy [162]. These are also used as alternative for corneal grafts and a biological matrix for limb cells cultures used to regenerate the corneal lesions. These cells remain viable and reconstruct a stable ocular surface. Similarly, cultivated oral mucosal epithelial transplantation (COMET) is used for treatment of eyes with total limbal stem cell deficiency [163]. However, for normal regeneration epithelialization of the corneal surface setting of micro niche and growth inducing factors are highly essential for lower down the transplantation failures and other complications [163]. By using explants cultures epithelial-mesenchymal transition can be made for intrastromal transplantations [164].
Stromal cell secreted soluble factors/ growth factors are used to establish micro-niche of corneal epithelial stem cells. But in vitro cultures epithelial cells organize to form epithelial clusters and make sheet like structures which upon dislodging by gentle enzymatic digestion separate into transplantable cell population [165]. Corneal limbal stromal progenitor cells are used as autologous cell source to produce functional neurons [166]. Limbal stromal niche cells heterogeneously express embryonic stem cell (SC) markers [159]. Both human corneal stromal stem cells (hCSSCs) and human corneal fibroblasts (hCFs) are used for generation of human corneal stromal tissue. hCSSCs successfully differentiated into keratocytes which form multilayered lamellae with orthogonally-oriented collagen fibrils [167]. Limbal stem cells are transplanted for restoration of corneal transparency. These are cultured on a highly-aligned fibrous substrate made from poly (ester urethane) urea. Similarly, corneal allotransplantations are also made by intravenous infusion of human MSCs (hMSCs) [168]. However, by homing of human umbilical cord blood mesenchymal stem cells in defective areas injured corneal endothelium can be restored [133]. MSCs are also to replace damaged or diseased corneal endothelium [133].
From hESCs, CECs can be derived similar to native human CECs [169]. These cells have potential application in replacement therapies as substitution for donor CECs [170]. Cultured human CECs show stem cell markers, including nestin, OCT3/4, and GFAP which differ according to the culture media and associated proliferation rate [172]. Adipose tissue derived mesenchymal stem cells show expression of epithelial markers i.e. CD34, CD90, p63, and ABCG2 and CK3/76, CK12, CK76, CK19, and CK1/5/10/14. These also display expression of putative stem cell markers (CD90, ABCG2, and p63) and cytokeratins (CK12 and CK76). These markers provide self-renewal capacity and intrinsic plasticity to adipose tissue derived mesenchymal stem cells. After cellular differentiation these cells acquire some epithelial-like characteristics. Due to their high self renewal capacity adult ADS cells are used as a potential source for cell therapy in ocular surface regeneration [171]. Mouse adipose tissue mesothelial cells (ATMCs) show similar morphologic and biochemical characteristics with mouse corneal endothelial cells (CECs). These show capacity to adhere to the decellularized basal membrane of human anterior lens capsules (HALCs) and are used as potential tissue-engineered source for corneal endothelium replacement [172] (Figure 2). Stem cells are also used to generate neogenetic structure from a lineage of bone marrow-derived mesenchymal stem cells [173]. Embryonic stem cell using stromal cell-derived induce cellular proliferation both in vitro and in vivo. Similarly, BM cell types may infiltrate into injured and/or diseased tissues and subsequently differentiate to form phenotypes of residential cells when injected. These cells are also used to repair damaged tissue sending via circulation to generate a keratocyte phenotype [153]. Periocular mesenchyme derived from the neural crest (NC) make mammalian eye, but signals which coordinate the formation of ocular structures are still unknown [174].
Corneal reconstruction by tissue bioengineering
Corneal reconstruction is among the most effective methods for curing corneal injury due to various clinical disorders [175]. Corneal epithelial stem cells (SCs) need more adaptable niche to differentiate into limbal palisades of Vogt, located between the cornea and the conjunctiva. But limbal stem cells also require close physical association with their native NCs via SDF-1/CXCR4 signaling for appropriate differentiation [157]. However, for management of corneal limbal stem cell deficiency Boston type I keratoprosthesis is followed [176]. Prior to CLSC transplantation anti-lymphangiogenic treatment is also required [177]. Surface treatment to a biomaterial surface modifies cell type and accelerates the cell growth [171]. However, for generation of complex organ structures mainly any eye component it will require the intricate orchestration of multiple cellular interactions. Few genes linked to Lhx2’s function in the expansion and patterning of progenitor cells have been identified [178].
Bioengineered corneas are used as prosthetic devices for replacement of the cornea and restoration of its functions. These are used with tissue-engineered hydrogels that allow regeneration of the tissue. Though there are difficulties of immune rejection and shortage of organ supply for corneal transplantation. Besides, natural keratoplasty, artificially developed cornea is also used to replace damaged one but it shows low biocompatibility. Hence, to meet out the shortage of donor corneas for transplantation, particularly in developing countries, bioengineered corneal tissues are used in form of explants for tissue therapy. Bioengineered corneas attribute near about similar transparency and compatibility natural corneas and with host cells. Bioengineered methods are developed and standardized for mass production of low-cost corneas. BPCs fabricated into hydrogel corneal implants provide over 90% transparency and four-fold increase in strength and stiffness compared with previous versions [179]. This is the main reason that tissue engineered corneal transplantations were found more successful to treat blinding diseases [180].
Corneal stroma is avascular connective tissue that is characterized by layers of highly organized parallel collagen fibrils which are mono-disperse in diameter with uniform local inter fibrillar spacing. Emulation of corneal stromal tissue is most challenging task in bioengineering to have artificial human cornea. It is very difficult to reproduce highly ordered microstructure, with all biomechanical properties and optical transparency of this tissue [181]. Therefore, both hCSSCs and RGD surface-coupled patterned silk film are used to develop highly ordered collagen fibril-based constructs for corneal regeneration and corneal stromal tissue repair [181]. Natural corneal stroma is used as an optimal substrate to construct a natural corneal equivalent to repair eye defects. For this purpose human corneal epithelium is cultured from donor limbal explants on corneal stromal discs that are prepared by FDA approved Horizon Epikeratome system. Morespecifcally, autologous rASCs are used as cell source for corneal stromal restoration. Mainly autologous rASCs-PLGA constructed corneas developed by following tissue engineering methods make transparent intact without corneal neovascularization [182].
More specifically, collagen vitrigel (CV) is used for reconstructing corneal epithelium in the stromal wound and limbal stem cell deficiency (LSCD) [183]. This collagen vitrigel is used as a scaffold material for for hLEC transplantation without having complications [183]. It supports corneal epithelial differentiation and prevents epithelial hypertrophy. Similarly, nanofibers prepared from copolymer PA6/12 represent a convenient scaffold for growth of LSCs and MSCs and transfer to treat SC deficiencies and various ocular surface injuries [184]. Moreoften, copolymer PA6/12 nanofibers displays stability in aqueous solutions, biocompatibility as good matrix that supports growth of LSCs, MSCs, and corneal epithelial and endothelial cell lines [184]. Similarly, Bombyx mori silk fibroin is also used as a substrate for human limbal epithelial (L-EC) and stromal cell cultivation. 3D engineered limbus constructed from B. mori silk fibroin, showed potential benefits in corneolimbal tissue regeneration [185]. Dual-layer fibroin scaffolds are also prepared by using L-EC and L-MSC secreted matrix and polylactic-co-glycolic acid (PLGA) for repairing corneal stromal defects [182].
Thus, bioengineered spatially complex, collagen-based nano-structured constructs are used for corneal repairing and regeneration [185]. Similarly, bioengineered synthetic corneal tissue derived from corneal stromal stem cells of human origin is also used as a quality biomaterial for corneal reconstruction [186]. Similarly, corneal epithelium is used to make tissueengineered hIDPSC sheet and reconstructs for transplantation in vitro experiments by maintaining limbal stem cells cultured onto human keratoplasty lenticules (HKLs). HKL is a suitable scaffold material to obtain natural corneal graft for clinical purposes [187]. It induces proliferation, express differentiation markers. It binds to the underlying stroma with no alterations in clonogenic potential. HKLs allow cell growth with no feeder layers, to be freeze dried, and to preserve the integrity and viability of stromal keratocytes [187]. Hevin is a matricellular protein that is used in tissue repair and remodeling via interaction with the surrounding extracellular matrix (ECM) proteins [188]. Hevin is transiently expressed in the IrrPTK-injured corneas. Its loss predisposes aberrant wound healing and generates severe chronic inflammation and stromal fibrosis. Hevin plays a pivotal role in the corneal wound healing [188]. Electrospin is used for making constructs using rabbit limbal epithelial and stromal cells [181]. It is a biodegradable membrane made up of poly(lacticco- glycolic acid) 50:50, which incorporates the features of the underlying microfabricated structures. More recently, tissueengineered hemicornea is also used for therapeutic purpose in patients which showed total limbal stem cell deficiency [133].
Today nonbiological corneal substitutes such as poly (ethyl acrylate) (PEA)-based copolymers, extracellular matrix-protein coating are used for increasing the survival rate of grafting tissues. Similarly, colonization with adipose-derived mesenchymal stem cells has also increased the survival rate of grafts. In addition, for obtaining good results and longer survival human adipose tissue derived mesenchymal stem cells (h-ADASC) and PEA-based copolymers are used in combination with extracellular matrix coatings and macroporous membranes composed of the optimal PEA subtypes and coating proteins. PEA with low hydroxylation as a scaffold also gave near good results [138]. Biological matrix is used for stem cell growth and transfer that could be possible by using co-culture system.
Patients with advanced corneal disease show very poor conventional corneal transplantation success and need keratoprosthesis (KPro) for visual rehabilitation. For contsruction of KPro is poly(methyl methacrylate) (PMMA) in the is used in central optical core and a donor cornea as skirt material [189]. Thin collagen matrix and fibroblast-like cells are used in keratoplasty mainly in repairing of retrocorneal membranes (RCMs). In addition, carrier materials such as collagen, fibrin, siloxane hydrogel, poly(ε-caprolactone), gelatin-chitosan, silk fibroin, keratin, poly(lactide-co-glycolide), polymethacrylate, hydroxyethylmethacrylate and poly(ethylene glycol) are potentially used for treatment of limbal stem cell deficiency [190].
Tissue-engineered cell sheets are used for ocular surface reconstruction in animal models mainly having total limbal stem cell deficiency (LSCD) [191]. These sheets are made by using human undifferentiated immature dental pulp stem cells (hIDPSC). For designing new tissue engineering scaffolds regulatory information available on cell signaling may assist in the long-term success of implants that can be used for reparing mechanically damaged ocular surface in the experimental animals [44]. In experimental animal models cornea is damaged by a variety of clinical disorders or chemical, mechanical, and thermal injuries. However, to prepare tissue engineered corneal substitutes (TEC) to treat corneal surface defects in a limbal stem cell deficiency model induced bone marrow mesenchymal stem cells (BMSCs) of corneal lineage are used [192].
Human corneal stromal stem cell (hCSSCs) when cultured on biodegradable poly(ester urethane)urea (PEUU) get differentiated to keratocytes. These are also used to produce abundant matrix, that helps in organization of the transparent connective tissue of the corneal stroma by differentiated keratocytes. Similarly, human mesenchymal stem cells (MSC), cultured without any feeder layer (NF) do derivatization of cornea epithelial that is used for making constructs mainly for xenografts [193]. MSCs cultured on nanofiber scaffolds provide protection from formation of toxic peroxynitrite. It lowers the apoptotic cell death and decreased matrix metalloproteinase and pro-inflammatory cytokine production which lower down corneal inflammation as well as neovascularization and significantly accelerated corneal healing [194]. Further, bioengineering technology has evolved new scaffolds /biomaterials which are used in reconstructing corneal epithelium. However, for promoting interactions between neurons and corneal tissue coculture methods are developed. There is an increasing demand of bioengineered corneal tissues for surface reconstruction and transplantation purposes. For this purpose new methods are being developed to supplement tissue donation and providing innovative opportunities to regenerate cornea tissue.
Conclusion
Corneal eye defects are commonly seen in old age and newly born babies. Common diseases of the cornea are keratitis, ocular herpes, herpes zoster and keratoconus. These conditions can damage the cornea, resulting in scars that interfere with vision by distorting light as it enters the eye. In Keratitis patients face sever inflammation, infection and ulceration of the cornea. Among important symptoms includes redness, blurred vision, discharge, severe pain, tearing and extreme sensitivity to light. Among important causes are problems in gene regulation or gene mutations, environmental stress, infection and injuries. Herpes zoster is a skin disease caused by chickenpox virus but it spreads to eyes and cause lesions on the cornea. Herpes simplex virus causes sores on the cornea and is not curable. Keratoconus causes scarring, swelling and changes the shape of the cornea, creating distortions such as nearsightedness. Moreover, congenital disorders originate during embryonic development could be partially restored or improved by stem cell transplantation therapy. But in old ages both stem cell therapy and organ derived sub-organelle transplantations with new co-polymer matrixes and hydrigels are used to reduce chances of therapeutic failures. In vivo transplantation of corneal stem cells induces visual tissue repairing and its regeneration. These should have enormous potential to treat various pathological conditions especially for corneal reconstruction. Transplantation of keratoplasts is the most effective method used for treatment for corneal blindness. But vascular regeneration of cornea by using certain cell growth induces and healers can easily cut down pain and its sensitivity in such patients. Furthermore, new biocompatible scaffold materials are also required for restoration of eye defects mainly for treatment of persistent epithelial defects. These scaffolds are used in corneal transplantation in patients facing Limbal stem cell deficiency (LSCD). Few important silk fibroin scaffolds, poly(ethyl acrylate) (PEA), polylactic-coglycolic acid (PLGA) are bioengineered also used for repairing corneal stromal defects. Cyanoacrylate glue is used to promote epithelialization and halt progression. The glue is useful in cases of perforations less than 2mm. This method is good alternative to avoid or delay corneal transplantation when the risk of graft rejection is high. For small- to intermediate-sized perforations, lamellar grafts have the advantage of lower rejection rates, faster healing times, and preservation of endothelium compared with penetrating keratoplasty. Fibronectin is a naturally occurring glycoprotein found in serum that promotes cellular adhesion in wound healing. Thymosin beta 4 (Tβ4) is a naturally occurring polypeptide secreted by inflammatory cascade cells. It plays an active role in promoting corneal wound healing. In clinical reports topical, non-preserved ophthalmic Tβ4 also known as RGN-259 is used for treatment of nonhealing neurotrophic epithelial defects. Topical ophthalmic Nexagon gel is applied for treatment of alkali corneal burns. Various stem cell types such as human corneal stromal stem cell (hCSSCs, bone marrow mesenchymal stem cells (BMSCs), immature dental pulp stem cells (hIDPSC), umbilical cord mesenchymal stem cells (UMSCs) are used for therapeutic purposes and treatment of cornea.
For more Open Access Journals in Juniper Publishers please click on: https://www.crunchbase.com/organization/juniper-publishers
For more articles in Open Access Global Journal of Intellectual & Developmental Disabilities please click on: https://juniperpublishers.com/gjidd/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/



Comments
Post a Comment